views
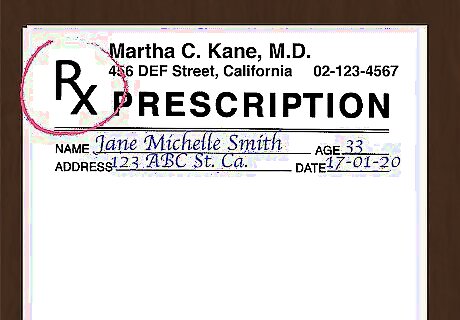
- Include the patient's full name and date of birth, your full name and contact information, the date of the prescription, and your signature.
- Write the name of the medication and the strength you're prescribing.
- Include the amount of medication that should be filled and the number of refills allowed.
- Add use directions for the medication, including the route, dosage amount, frequency, and when to discontinue use.
Basic Information
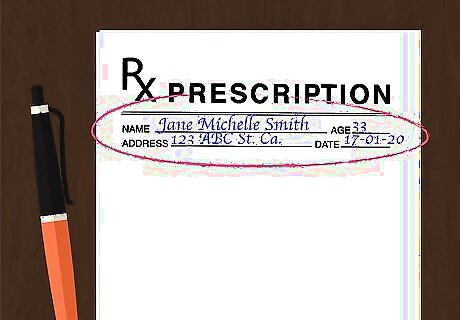
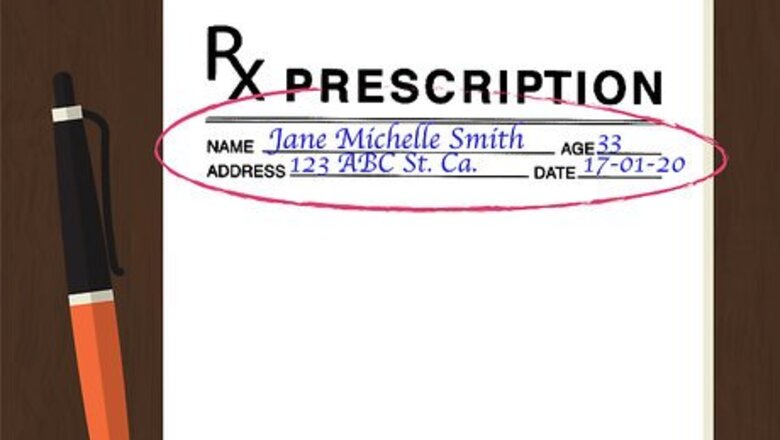
Include at least two patient identifiers. Patient identifiers are pieces of information used to clarify the identity of the patient. In all settings, you must include at least two of these identifiers. Full name and date of birth are the two most common identifiers. For prescriptions fulfilled outside of a hospital, the patient's phone number and/or current home address will usually be included, as well. One identifier isn't enough, even if you use the patient's full name. If two patients share the same name, it would be impossible to know which one the prescription refers to without any other identifier.
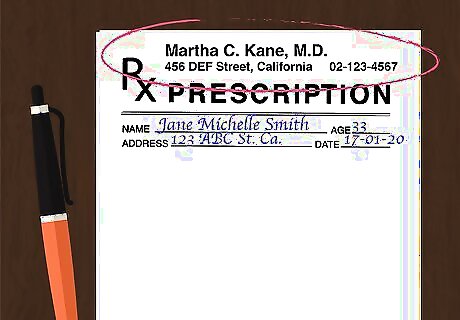
Provide your information. As the prescriber, your name and contact information must also be listed on the prescription. Include your full name, the address of your medical practice, and the phone number of your medical practice. Note that your United States Drug Enforcement Administration (DEA) number must also be included somewhere on the prescription. In most cases, this information will already be printed on the prescription form. If it isn't, however, you will need to write it manually.
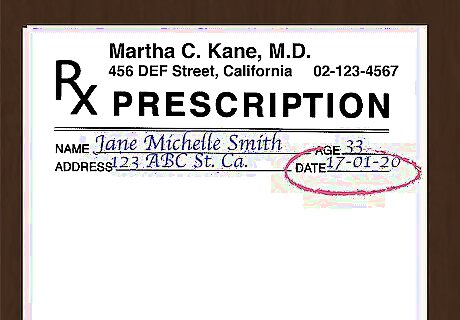
Note the date of the prescription. Some prescriptions must be filed within a certain time period. Even when the medication being prescribed does not fall into that category, you should still include the date. Time-sensitive drugs are rated based on schedule categories. Schedule I drugs have a high potential for abuse and have no legally accepted medical use within the United States. Schedule II drugs have a high potential for abuse but do have some legally accepted medical use. Schedule III drugs have some potential for abuse and can be used for some medical purposes. Schedule IV drugs have a relatively low potential for abuse and are legally permitted for some medical purposes. Schedule V drugs have an even lower potential for abuse and are legally permitted for certain medical purposes.

Sign the prescription. You will need to sign each prescription before it can be considered valid. Your signature will usually go at the bottom of the form, regardless of whether or not there is a specific line for it there. It is strongly recommended that you write out the rest of the prescription and sign your name last. Doing so prevents unfinished or blank prescriptions from falling into the wrong hands.
Inscription
Display the "Rx" symbol. "Rx" is the symbol for "superscription." Write it just before you write out your instructions for the medication itself. On most prescription forms, the "Rx" is already printed. Write the inscription information immediately after this symbol. The inscription includes all of the information about the specific drug you want to prescribe.
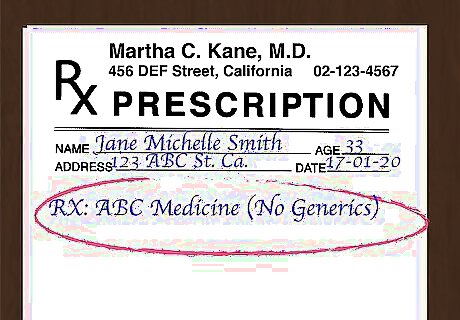
Write the medication. You should typically use the generic, non-proprietary name of the drug instead of the name brand. Use the name brand of the drug only when you specifically wish to prescribe the name brand. Keep in mind that doing so may make the prescription more expensive for the patient. If you want to prescribe the name brand, you should also include a note on the prescription reading "No Generics." On most prescription forms, there will be a "Brand Name Only" or "No Generics" box you have the option of checking for this purpose.
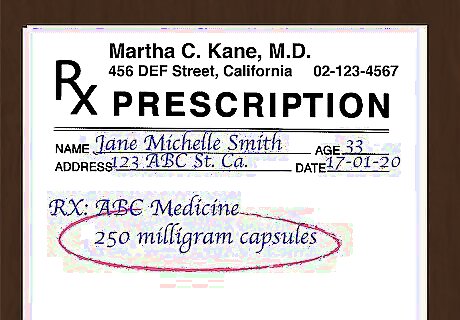
Mention the strength. Most medications come in multiple strengths, so you must mention the strength you wish to prescribe immediately after the name of the medication. The strength amount should be indicated in milligrams for tablets and suppositories and milliliters for fluids. Write words instead of abbreviations to avoid possible misunderstandings.
Subscription
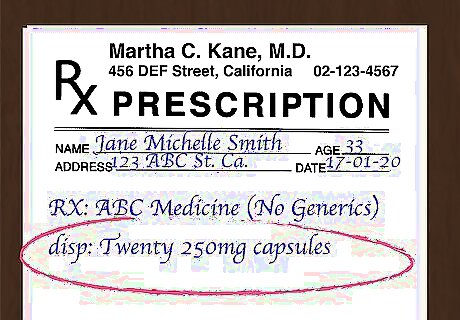
Include the prescription amount. Tell the pharmacist exactly how much of the medication should be filled and passed to the patient. This information should usually be preceded by an appropriate heading, such as "dispense," "disp," "#," or "how much." Include the specific bottle size or number of tablets/capsules. Spell the numbers out to avoid possible miscommunication.
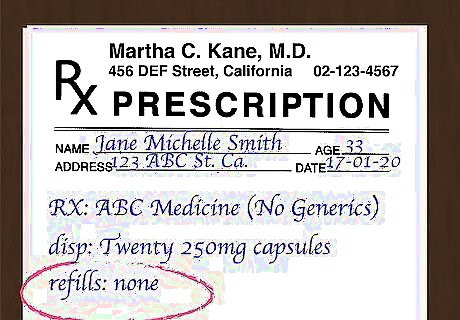
Note the number of permitted refills. For medications that treat a chronic condition or other similar reasons, you may wish to permit a certain number of refills before another prescription will be required. Only allow additional refills when the patient will need the exact same prescription multiple times. For example, you might wish to prescribe a year's worth of oral contraceptives, yet each fulfillment of the prescription might only provide a month's worth. On the prescription form, write "Refills 11" to indicate that eleven refills are permitted after the first fulfillment. After the final refill runs out, the patient will need a new prescription before any additional medication can be obtained. If you do not wish to permit any refills, write "Refills 0" or "Refills none" to indicate as much. Doing so reduces the risk of possible tampering.
Patient Use Directions
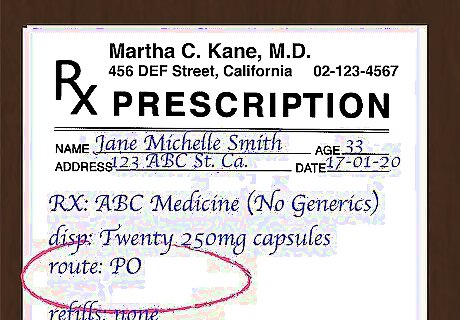
Specify the route. The route is the method used to take the medication prescribed. When writing the route, you can mention the instructions using either the accepted English term or the corresponding Latin abbreviation. Common options include: By mouth (PO) Per rectum (PR) Intramuscular (IM) Intravenous (IV) Intradermal (ID) Intranasal (IN) Topical (TP) Sublingual (SL) Buccal (BUCC) Intraperitoneal (IP)

State the dosage amount. State how much of the medication the patient should use each time he or she takes it. These instructions will be transferred to the prescription label once it is fulfilled. For instance, you might write something like "one 30 milligram tablet" or "30 milliliters.
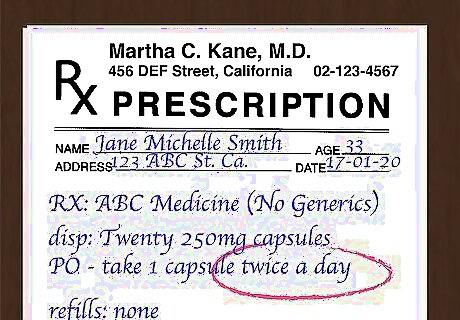
Indicate the frequency. The frequency describes when and how often the medication should be taken. It is strongly recommended that you write out the frequency in full rather than using abbreviations. In fact, a medication that must be used "daily" or "every other day" must be written out in full. Abbreviations for these frequencies are prohibited. Other frequency abbreviations can be used, but it is still recommended that you spell out the instructions instead of using the abbreviated form. Several common options include: Twice a day (BID) Three times a day (TID) Four times a day (QID) Every bedtime (QHS) Every four hours (Q4H) Every four to six hours (Q4-6H) Every week (QWK)
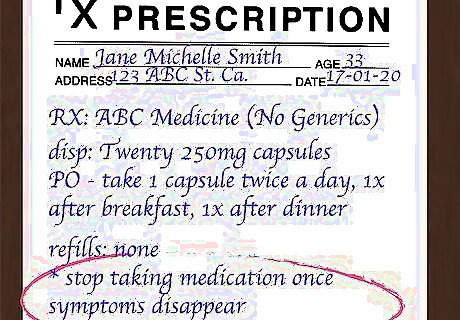
Write when to discontinue use. Most medications must be taken until the drug runs out. In some cases, however, the patient should stop taking the medication once his or her symptoms disappear. You should specifically write which is the case on the prescription form.

Consider including the diagnosis. When a medication should only be used on an "as needed" basis, you should include a brief diagnosis or reason for taking the medication. Specify this diagnosis with the abbreviation "PRN." For example, the statement for a pain medication might read "PRN pain."
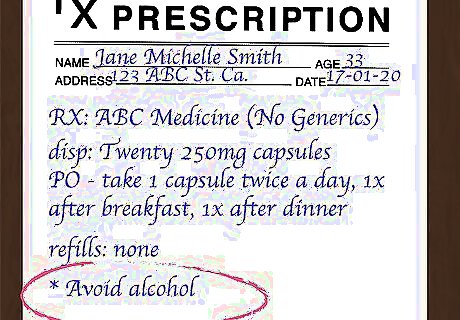
Mention any other special instructions. Occasionally, there might be a special instruction that needs to go on the label. Let the pharmacist know to include it by specifically writing the instruction on the prescription form. A few common examples include: "Take with food" "Avoid alcohol" "Keep refrigerated" "Do not freeze" "For external use only" "Shake before instillation"
















Comments
0 comment