views
India’s steady economic growth has, by and large, led to an improved standard of living for its people. In particular, cities and urban centres have become more affluent, and the lifestyles of city dwellers increasingly resemble those of their counterparts in western countries. This affluence and growth is accompanied by the eradication of several diseases that arose from malnutrition, poor sanitation, unhygienic food and water.
But, there is a flip side. Increased affluence, increased urbanisation, sedentary lifestyles and richer food bring with them a number of lifestyle diseases – obesity in particular, especially in children1. Obesity tends to bring with it high blood pressure and diabetes2.
In India, the total number of people with diabetes was estimated to be 77 million in 2019, 43.9 million of whom were undiagnosed. Globally, one in two adults living with diabetes, (overwhelmingly type 2 diabetes, aged 20–79 years) are unaware that they have the condition3.
These numbers are estimated to rise. According to the International Diabetes Federation Atlas 2019, the number of people with diabetes will rise to 101 million in 2030 and to 134 million in 20453. For a country where medical services are already stretched thin, this could prove to be a difficult burden. Diabetes brings with it a host of complications as it affects nearly every organ system in the body – people with diabetes are more prone to problems with the kidneys, the lower limbs, and even the eyes.
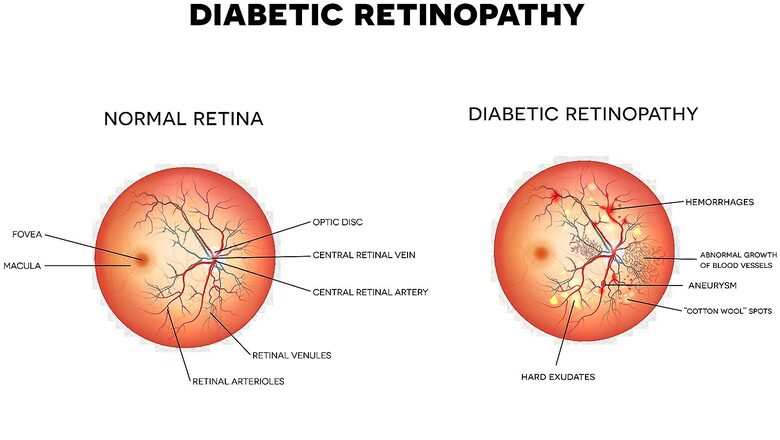
Diabetes has become the fifth leading cause of blindness across the globe4. DR is one of the major reasons for visual impairment and blindness among people with diabetes across the globe3. DR is also acknowledged to be one of the leading causes of blindness in the working age population with devastating personal and socio-economic consequences3.
It is also known as a silent thief of sight: No pain. No vision changes. No clues at all. In fact, according to Dr Manisha Agarwal, Joint Secretary, Retina Society of India, one of the earliest symptoms is a persistent difficulty in reading that doesn’t go away even with a change in spectacles. This means that by the time you begin to see symptoms, irreversible damage to vision has already occurred2. However, once diagnosed, vision loss due to DR can be stopped in its tracks with the right interventions5. Diagnosis involves a DR eye test administered by an ophthalmologist. People with diabetes need to get themselves tested for DR annually6.
The awareness gap
DR affects nearly 18% of people with diabetes in India. That’s almost 1 in 5 people with diabetes3. In a Roundtable Discussion in Season 1 of the Netra Suraksha Initiative, Dr Dinesh Talwar, Director in Virtreoretinal and Uveal Disorders at the Centre for Sight in New Delhi, drew attention to the fact that that people are not aware that they need to come regularly for screening for DR, and that lack of awareness creates a challenge in battling DR at a societal level. Think about any of the people with diabetes in your family and social circles – have you ever had a conversation about Diabetic Retinopathy?
This is sobering. DR largely affects those in the working age group of 20-70 years of age3, which means that those families where the primary breadwinner is a person with diabetes are also made financially vulnerable, when such people suffer from DR. The good news is that vision loss from DR is largely preventable, provided one is diagnosed early, and works closely with their doctor to manage the disease5.
Network18 has launched the ‘Netra Suraksha’ – India Against Diabetes initiative, in association with Novartis, to spread awareness about DR to the people most likely to be affected by it. The initiative aims to spread awareness about DR through informative articles and in person check up camps. We hope that once people with diabetes are made aware of this vulnerability, they will take steps to get themselves and their loved ones tested for DR and for diabetes regularly.
The physician gap
However, the next hurdle in the battle against DR in India, is the shortage of trained ophthalmologists. Currently, India has about 12000 ophthalmologists (roughly 3500 retina specialists). The shortage of retina specialists is particularly acute – just 1 retina specialist per 1.26 million people7. When we compare the number of ophthalmologists (12000) to the number of people with diabetes (over 100 million people with diabetes by 2030), the number climbs to 1 ophthalmologist for every 8,333 people with diabetes. Considering that people with diabetes need to test their eyes annually for DR, India is woefully short on physicians.
This is a problem that needs to be solved at a policy level, as the gap between the demand and supply here is only going to widen with time. There have been interesting developments using AI powered fundus cameras that automate the screening of DR. Increased adoption of this technology should also help narrow the gap.
The economics of the disease
DR is increasingly occurring in younger populations as diabetes (especially Type 2) is increasingly occurring in younger populations. While loss of vision harms a person’s earning capacity at any age, when it happens early, it hurts their ability to build up a retirement corpus, their families are probably younger (and the children are still studying), and their earnings are still low. Loss of vision also brings with it several unforeseen expenses – the need for an attendant, rehabilitation and training costs, reskilling costs and so on.
The most direct expenses though, are medical ones. When one develops sight threatening DR, the symptoms become hard to ignore. This is followed by a number of doctor’s visits, tests, interventions and medications. Depending on where the person is located, the costs can spiral. If located in a metropolitan city, medical expenses can be daunting. If located in a small town or rural part of the country, the person may have to travel to a larger city, and their medical bills are compounded with travel and boarding costs.
Insurance can help, provided one doesn’t develop DR or any diabetes related complications in the waiting period. Most insurers institute a long waiting period (often spanning years) for diabetes related complications. Diabetes specific insurance policies don’t have waiting periods, but they too, have certain exclusions. This means that even if the person has an insurance product that is geared towards people with diabetes, it may not cover all the costs.
The costs of insurance for people with diabetes are only going to rise. The number of diabetes-related claims has risen by 120% between 2016 and 2019. The sharpest rise in absolute terms has been in the 20-30 age-bracket8. Traditionally, where we see these trends, insurance premiums get more expensive.
Prevention is better than cure
With all these challenges at play, what can a person with diabetes do to better care for their vision? For starters: begin screening your blood sugar, and work with your doctor to gain better metabolic control. This means looking after several markers – your blood pressure, serum lipid levels, mineral and vitamin deficiencies, and of course, the trifecta of diet, exercise and weight management5.
Second, get yourself an insurance policy that is geared towards helping people with diabetes. Then, educate yourself on the inclusions and exclusions. Understand the waiting period, and read all the fine print. The more you know now, the better your decision making will be when you need it.
Third, set your annual ophthalmologist appointment for screening DR and don’t miss it. DR is asymptomatic in the early stages, and the earlier you catch it, the better your prognosis.
Finally, educate yourself on everything to do with DR. A good place to start is the Netra Suraksha Initiative website where you can find in-depth panel discussions, videos, and knowledge articles. Be your own champion, and encourage others in your circle to be champions for their vision.
Source:
- Countries in transition: underweight to obesity non-stop? Available at: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002968 [Accessed 8 Sep 2022]
- Patel SA, Ali MK, Alam D, Yan LL, Levitt NS, Bernabe-Ortiz A, Checkley W, Wu Y, Irazola V, Gutierrez L, Rubinstein A, Shivashankar R, Li X, Miranda JJ, Chowdhury MA, Siddiquee AT, Gaziano TA, Kadir MM, Prabhakaran D. Obesity and its Relation With Diabetes and Hypertension: A Cross-Sectional Study Across 4 Geographical Regions. Glob Heart. 2016 Mar;11(1):71-79.e4. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4843822/#:~:text=Every%20standard%20deviation%20higher%20of,%2C%20aged%2040%E2%80%9369%20years. [Accessed 25 Aug 2022]
- IDF Atlas, International Diabetes Federation, 9th edition, 2019. Available at: https://diabetesatlas.org/atlas/ninth-edition/ [Accessed 5 Aug 2022]
- Pandey SK, Sharma V. World diabetes day 2018: Battling the Emerging Epidemic of Diabetic Retinopathy. Indian J Ophthalmol. 2018 Nov;66(11):1652-1653. Available at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6213704/ [Accessed 5 Aug 2022]
- Complications of Diabetes. Available at: https://www.diabetes.org.uk/guide-to-diabetes/complications [Accessed 3 Aug 2022]
- Raman R, Ramasamy K, Rajalakshmi R, Sivaprasad S, Natarajan S. Diabetic retinopathy screening guidelines in India: All India Ophthalmological Society diabetic retinopathy task force and Vitreoretinal Society of India Consensus Statement. Indian J Ophthalmol [serial online] 2021;69:678-88. Available at: https://www.ijo.in/text.asp?2021/69/3/678/301576 [Accessed 6 Sep 2022]
- Vashist P, Senjam SS, Gupta V, Manna S, Gupta N, Shamanna BR, Bhardwaj A, Kumar A, Gupta P. Prevalence of diabetic retinopahty in India: Results from the National Survey 2015-19. Indian J Ophthalmol. 2021 Nov;69(11):3087-3094. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8725073/ [Accessed 5 Aug 2022]
- Diabetes health insurance is expensive. Here’s a 4-point guide to manage related costs Available at: https://economictimes.indiatimes.com/wealth/insure/health-insurance/diabetes-health-insurance-is-expensive-heres-a-4-point-guide-to-manage-related-costs/articleshow/71982198.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst [Accessed on 5th, August, 2022]
This is a partnered post.
Read the Latest News and Breaking News here



















Comments
0 comment