
views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
Although heart palpitations can be a worrisome or a strange experience, they're usually harmless. In most cases, it's possible to find the cause and address it in order to reduce palpitations.
Lifestyle Changes

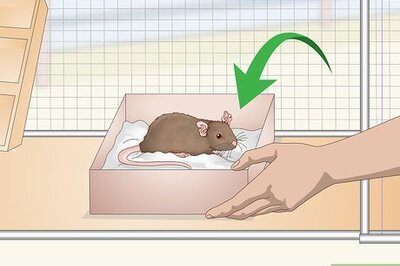
Rest and take a break. Some people experience heart palpitations due to physical overexertion or being too active; however, an increased heart rate from exercise or anxiety (called tachycardia) is not the same as palpitations. Both can happen at the same time, although palpitations are defined best as unusual heart beats, not just fast heart beats. If your palpitations seem to be sometimes triggered by exercise, then stop what you're doing and rest for five to 10 minutes and catch your breath. Alternatively, reduce your exertions or change your exercise to something less strenuous. Walk instead of jogging, for example. Lift smaller weights. Gently tread water in the pool instead of doing strokes. Resting heart rates vary between people, but it's typically between 60 and 100 beats per minute. Palpitations can occur above, below or within the normal heart beat range.
Reduce your stress/anxiety. Moderate-to-high levels of stress and anxiety are relatively common triggers for heart palpitations due to the release of too much "stress hormones" into the bloodstream.hus, you may be able to prevent or reduce your palpitations by managing how you react or respond to stressful situations. Stress-relieving techniques like yoga, tai chi, deep breathing, visualization, meditation, biofeedback and aromatherapy are all helpful for promoting relaxation and better heart health. Ask at your local gym, community center, church or health clinic about joining a yoga or tai chi class. Taking deep breaths can naturally lower your heart rate and reduce the occurrence of heart palpitations, especially if you practice positive visualizations or guided imagery. Buy some relaxing aromatherapy candles (lavender scented, for example) and light them in the evenings prior to going to bed. Don't forget to get enough sleep — at least eight hours per night, although some people need a little more. A chronic lack of sleep can lead to anxiety and heart palpitations. Remove yourself from stressful situations, such as arguments. Quit focusing on financial problems. Stop watching scary movies or shows.
Avoid consuming stimulants. There are a number of substances that affect your central nervous system (CNS) and can trigger heart palpitations, including alcohol, caffeine, nicotine, illicit drugs (such as cocaine and amphetamines) and some over-the-counter medications (particularly cold and cough medicines). Thus, if you're having periodic heart palpitations, consider what you're putting into your body on a regular basis, because it could very likely be the cause. Cut back on caffeine. Rich sources include coffee, black and green teas, most soda pop (especially colas), energy drinks and chocolate. Stop smoking. Nicotine from cigarette smoking can increase your resting heart rate up to 15 beats/min and increase blood pressure up to 10mm Hg. Stop binge drinking. Alcohol is actually a CNS depressant instead of a stimulant, but binge drinking often increases heart rate and chronic alcoholism tends to cause fluctuations (from too high to too low). Always check the ingredients of over-the-counter medications. Some cold and allergy remedies contain decongestants (such as pseudoephedrine), which can precipitate palpitations.
Vagal Maneuvers

Try the Valsalva maneuver. Vagal maneuvers are simple actions that you can do at home to affect your vagus nerve, which is the primary one that regulates your heart rate. Vagal maneuvers can slow your heart rate down and stop palpitations within seconds if done correctly. The Valsalva technique involves holding your breath and bearing down as if you're having a bowel movement for about 15– 20 seconds — it increases your intrathoracic pressure and stimulates the vagus nerve. The Valsalva technique can change the rhythm of electrical impulses in your heart, help your heart rate return to normal and reduce palpitations. The Valsalva maneuver shouldn't be done if you have heart disease or are advanced in age, as it may increase the risk of stroke.

Activate your diving reflex. The diving reflex gets activated when your head or face gets cold for more than a few seconds — your heart rate slows down to reduce blood flow in an attempt to survive, which is helpful when submerged in cold water. To trigger this survival reflex, place very cold water or an ice pack against your face for about 10 seconds. Your heart rate and palpitations should reduce pretty quickly. Dip your face or submerge your head in cold water. Put a wet face cloth in the freezer for 30 minutes then press it against your face. Alternatively, drinking a glass of very cold water will cool the hard palate of your upper mouth and also mildly trigger the diving reflex. Vagal maneuvers are simple and generally quite safe to do, but they should be done as soon as you realize you're experiencing palpitations for best results. Do not attempt vagal maneuvers while standing — they can sometimes cause dizziness and fainting.

Try coughing a bunch of times. You can also try coughing forcefully (or clearing your throat) multiple times in efforts to move your diaphragm, increase intra-thoracic pressure, and stimulate your vagus nerve. In essence, coughing creates the same physiological effects as bearing down (the Valsalva technique), but some people may find it easier to perform. When coughing, it must be forceful enough and sustained — a single, light cough won't likely trigger a vagal response. Make sure to completely swallow any food you're eating or beverages you're drinking in order to prevent the risk of choking. If you're unsure, ask your doctor for a demonstration of vagal maneuvers.
Getting Medical Attention

Make an appointment with your doctor. Although heart palpitations are not considered a serious condition and seldom require treatment, sometimes they can be caused by heart disease. If you're experiencing regular palpitations for more than a few days or periodic palpitations for more than a few months, make an appointment with your doctor to get your heart checked out. Palpitations could be caused by something as simple as stress, but they could also be signs of developing an irregular heart rhythm such as atrial fibrillation, which is a huge risk factor for having a stroke. Your doctor will give you a physical exam, check your heart rate and listen to your heart with a stethoscope. Your doctor will likely order an EKG (electrocardiogram) to check your heart's electrical activity. Even if your EKG results are normal, you still can have a medical condition that's causing palpitations. You may get a referral to a heart specialist (cardiologist) and be told to wear a Holter or event monitor, which records your heart’s electrical activity for up to 48 hours You may also get an echocardiography (ultrasound image of your heart) and/or a stress test (monitored intense exercise) to try and find the cause of your palpitations.

Talk to your doctor about drug side effects. Some medications, particularly when they are combined with others, can trigger a racing heart (tachycardia) and/or palpitations. For example, anti-arrhythmic drugs (used to treat abnormal heart rhythms), digitalis, asthma medications, thyroid drugs, steroid therapy and most cold/cough remedies commonly trigger faster heart rates. Ask your doctor if your prescription medication(s) could trigger palpitations as an unwanted side effect. It's virtually impossible to predict how more than two drugs (taken concurrently) may interact with each other in your body, so read the list of side effects very carefully. If you suspect a drug is triggering your palpitations, don't stop taking it "cold turkey" without the supervision of your doctor — it may cause you worse symptoms. It's better to wean yourself off a drug and then switch to another with similar actions.
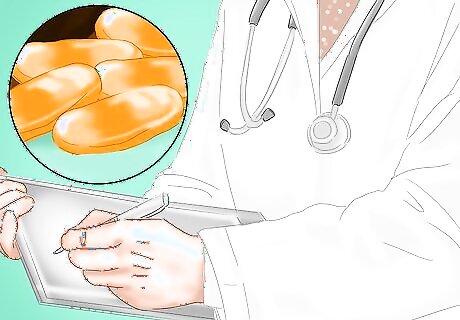
Ask your doctor about helpful medications. Although most cases of palpitations are harmless and either go away on their own or stop when the trigger is found, sometimes medication may be needed. Potential causes of palpitations (and tachycardia) that require medicine include: cardiomyopathy, congestive heart failure, myocarditis and heart valve disease. Anti-arrhythmic medications (amiodarone, flecainide, propafenone, dofetilide, ibutilide, quinidine, disopyramide, lidocaine, procainamide, sotalol, amiodarone) quickly reduce heart rates, especially if they are given via injection. Other medications that may be prescribed (and often used along with anti-arrhythmics) include calcium channel blockers (diltiazem, verapami) and beta blockers (metoprolol, esmolol, atenolol). People with atrial fibrillation (the most common type of arrhythmia) may be treated with blood-thinning medicines to prevent blood clots, such as: warfarin (Coumadin), dabigatran, heparin or aspirin.















Comments
0 comment