
views
Here are 10 tips for communicating better with your patients.
Don’t ignore basic pleasantries.
Greet your patients with a smile and their name when you see them. Never underestimate the power of small talk. Establish a human connection the moment you walk into the room. Smile, say hello, and shake your patient’s hand. Establish positive energy in the room to set the tone for how your conversation will go from there. For instance, you could walk into the room and smile and say something like, “Hi Chris! It’s good to see you again, how are you doing today?”
Take your time, even if you’re in a rush.

Give them the time and respect they deserve. You probably have a million things on your mind and other patients you have to see right after you leave the room. But while you’re in there, give your full attention to the patient you’re talking to. Avoid checking your watch or reaching for the door handle while they’re talking. It could irritate or upset your patient, especially if they’re concerned or worried about their health. Try to make your patient feel like they’re the center of the universe and the only patient you have to see that day when you’re with them.
Explain things as simply as you can.

Imagine how you would explain it to a middle-schooler. While your patients aren’t dumb, try to avoid overloading them with a ton of medical jargon and terminology. Use plain, simple language so they can better understand the information you’re giving them. For instance, instead of saying myocardial infarction, you can simply say heart attack. You can also use colloquial terms like ticker (for heart) or noggin (for head).
Ask your patients if they understand everything.

Make sure they know exactly what you’re telling them. After you explain a diagnosis or procedure, ask your patient to parrot it back to you. Listen to how they explain it in their own words and gently correct any mistakes that they make. Answer any questions that they have as well. Make sure they have a clear idea of what’s going on. This can be really important for complicated or rare diseases that are difficult for a non-medical person to understand.
Collaborate with your patients.
Talk about your recommendations and ask them what they think. Instead of simply explaining what’s going on and what you want to do to fix it, think of your relationship with your patient as a partnership. Tell them what you think are the best options and explain the pros and cons of each. Ask them what they think about it. Many patients may respond more positively if they feel like their input is valued. For instance, you could say something like, “So, we could always operate and try to fix the issue, but we could also give it some time to see if it heals on its own. Both are viable options, what are you leaning towards?”
Talk to your patient about their lives, too.
Informal conversation can be a useful diagnostic tool. Use small talk and personal stories as opportunities to extract pertinent medical info. Ask your patients about their families and what’s going on in their life. At the same time, slip in medical questions and listen to what they have to say. Demonstrate that you’re interested in not only their cases but their lives, which can make them trust you more and accept your recommendations. For example, you could ask a patient about any exercise they’ve done or sports they’ve played recently and then ask if they felt any pain or discomfort during the activity. You could also ask about your patient’s family to learn more about their medical history. For instance, you could say something like, “How about your father? Did he ever have any trouble with his heart or did he ever complain about being tired often?”
Look your patient in the eyes and listen to them.
Let them talk and pay attention to what they have to say. Avoid glancing at your watch or the clock on the wall. Give your patient your undivided attention and look them directly in the eyes to show them you’re listening. Try not to interrupt them when they talk either. Studies suggest that if a doctor lets a patient speak uninterrupted for 3-4 minutes, they’ll tell you up to 90% of what’s wrong with them. Plus, they’ll feel more valued and like you care about their well-being.
Avoid being judgmental.
Show empathy both verbally and nonverbally. It’s totally normal to feel a little frustrated if a patient is being stubborn or making poor choices. But it’s important to try to understand where they’re coming from and avoid saying or doing things that make them feel uncomfortable or like they can’t be honest with you. Be calm and understanding at all times when you talk to your patients. You want your patient to feel comfortable telling you everything, even if it isn’t good news or the best behavior. For instance, don’t get upset if they tell you they’ve been smoking or taking drugs.
Use the acronym AMEN for really sick patients.
Affirm, meet, educate, and no matter what, assure them (AMEN). Sometimes, you may have to deliver really difficult news that may be hard for your patient to handle or accept. But you can empathize with them and offer them hope without promising a miracle that may never happen. Validate their position by affirming their belief that things will get better and meet them on their level so they feel that you understand them. Educate them on the potential outcomes so they’re aware of the medical information and assure them that you’re committed to caring for them. For example, you can affirm their belief by saying something like, “I’m hopeful for a miraculous recovery, too.” and then assure them by saying something like, “I’ll be here for anything you need.”
Take advantage of technology.
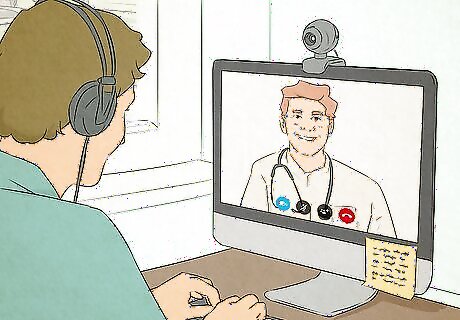
Use communication tools to stay in touch with patients. With events like the COVID-19 pandemic, doctors and medical staff have had to adapt and use a variety of technologies to communicate with patients and their families. Choose tools that work for you, such as Zoom or medical messaging apps like OhMD. Learn how to use them and show your patients how to use them so you can communicate through them if it’s necessary. Your hospital or medical network may use specific programs to communicate with patients. Learn how to navigate and use them so it’s easy for you to stay in touch.



















Comments
0 comment