
views
X
Expert Source
Ni-Cheng Liang, MDBoard Certified Pulmonologist
Expert Interview. 23 October 2020.
It may also be done in an emergency due to a blocked throat from an allergic reaction or growing tumor. Tracheotomies can be temporary or permanent. Caring for a permanent tracheostomy requires lots of knowledge and attention, particularly for infant patients and their caregivers while at home from the hospital. Make sure that you receive thorough training from the ENT or pulmonologist who placed your tracheostomy before attempting to care for it at home.[2]
X
Expert Source
Ni-Cheng Liang, MDBoard Certified Pulmonologist
Expert Interview. 23 October 2020.
This article is based off an interview with our board certified pulmonologist, Ni-Cheng Liang, MD. Check out the full interview here.
Suctioning the Tube

Gather your materials. Suctioning the tracheostomy tube is important because it helps to keep the airway free of secretions (mucus), which enables the patient to breathe better and reduces the risk of lung infection. Lack of proper suctioning is a major cause of infection in people who have a tracheostomy tube. The materials needed include: A suction machine Catheters (tubes) for suctioning (size 14 and 16 are used for adults) Sterile latex gloves Normal saline solution Normal saline lavage that is already prepared or a 5ml syringe A clean bowl filled with tap water

Wash your hands thoroughly. Caregivers (either at the hospital or at home) must wash their hands before and after tracheostomy care. This primarily protects the patient from getting a bacterial infection through his neck hole. Wash your hands with warm water and soap for at least 20 seconds and don't forget to scrub between your fingers and underneath your fingernails. Dry your hands using paper towels or a clean cloth. Turn off the tap using the paper towel or cloth as a barrier to avoid contaminating your hands again. As an alternative, lather your hands with an alcohol-based sanitizer and then let them air dry.
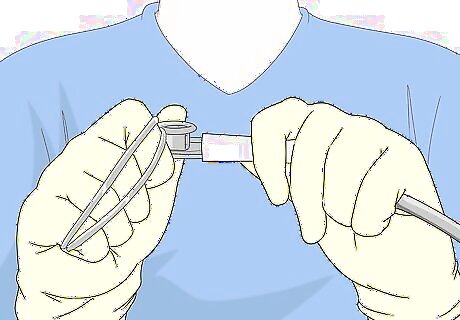
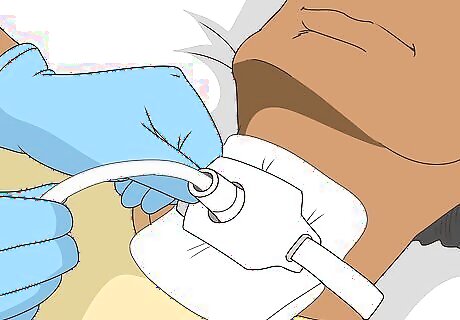
Prepare and test the catheter. Place gloves on hands. The suction machine package should be opened carefully, while taking care not to touch the tip of the catheter. However, the thumb control vent that is located at the end of the catheter can be touched, so don't worry about that. If you wind the catheter around one hand, it will keep it managed, freeing up your other hand for other tasks. The catheter is usually attached to suction tubing that is connected to the suction machine. Turn the suction machine on and test through the catheter tip whether it's able to suction. Test for suction by placing your thumb over the port of the catheter and releasing. A tracheal tube may have a single or double opening, and it may be cuffed or uncuffed, fenestrated (allowing for speech) or unfenestrated.

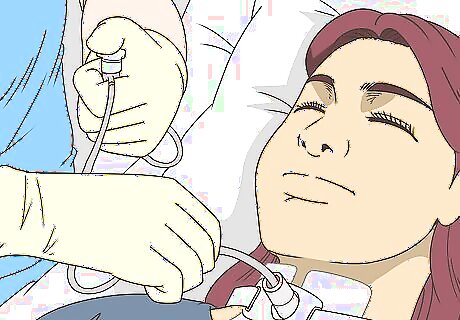
Prep the patient and administer saline. Make sure the patient’s shoulders and head are slightly elevated. She should be comfortable during this procedure. Have her take approximately three to four deep breaths to calm down. Once the patient is situated, put 3–5 milliliters (0.10–0.17 fl oz) of saline solution into the tracheal tube. This will help stimulate coughing up of mucus and add moisture to the mucus membranes. Saline solution should be used regularly while suctioning to prevent the formation of thick mucus plugs within the trachea, which can block the passage of air. Talk to the patient's healthcare professionals before you suction their tube. The care sometimes depends on the type of tracheostomy tube that's in place. The number of times saline should be instilled varies from one person to another depending on how thick or how much mucus she produces in her trachea. Caregivers should observe the color, odor, and thickness of the mucus secretions in case there's an infection — the mucus turns a grayish green and smells bad.
Insert the catheter and apply suction. Guide the catheter gently into the tracheal tube until the patient begins to cough or until it stops and cannot go any further. This should be approximately 4 to 5 inches (10.2 to 12.7 cm) deep into the tracheostomy tube in most cases. The natural curve of the catheter should follow the curve of the tracheal tube. Think of the catheter as a vacuuming device for cleaning the tracheal tube.The catheter should be pulled back a little before suction is applied, which should make the patient more comfortable. Apply suction by covering the thumb control vent while withdrawing the catheter from the tracheal tube in a slow and circular motion. Suction should not be applied for longer than about 10 seconds, during which the catheter should be rotating and pulling out consistently. There should always be suction on the way out. Tracheostomy tubes come in several sizes and materials such as semi-flexible plastic, rigid plastic, and metal. Some tubes are disposable, while others are reusable.
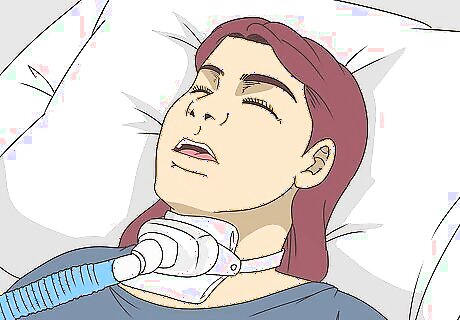
Let the patient get some air. Have the patient take three to four slow and deep breaths in between suctioning sessions because while the suctioning machine is working very little air can get to his lungs. The patient should be given oxygen after every suctioning is done or given time to breath depending on the patient's condition. With the catheter removed, suction tap water through the tube to get rid of any thick secretions, then wash the catheter with hydrogen peroxide. Repeat the process as needed if the patient is producing more secretions that have to be sucked out of the tracheal tube. Suctioning is repeated until the airway is clear of mucus/secretions. After suctioning, the oxygen is returned at the flow rate level that it was before the procedure.
Cleaning the Tracheal Tube

Gather your materials. It is important to keep the tracheal tubes clean and free of mucus and foreign debris. It's advisable to clean them at least twice a day — once in the morning and once in the evening is ideal. However, the more frequent, the better. Here's what you need: Sterile saline Half-diluted Hydrogen Peroxide (½ portion water mixed with ½ portion hydrogen peroxide) Small, clean bowls Small, fine brush

Wash your hands. It is essential that you wash your hands and remove all germs and dirt. This will help prevent any infection due to unhygienic care. The proper procedure for washing your hands is discussed above. The most important things to remember are to use a mild soap, lather your hands well, rinse them, and dry them with a clean, dry towel.
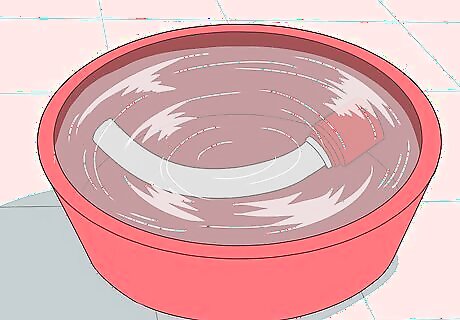
Soak the inner cannula of the tracheal tube. In one bowl, place the ½ strength hydrogen peroxide solution, and in another bowl the sterile saline solution. Remove the inner cannula of the tracheal tube carefully whilst holding the neck plate still, which should be taught by your doctor or nurse while in the hospital. Place the cannula in the bowl containing hydrogen peroxide solution and let it soak completely until the crusts and particles on the tube are softened, dissolved and removed. Some tracheal tubes are disposable and don't need to be cleaned if you have replacements.

Clean the inner cannula. Using a fine brush, clean the inside and outside of the inner cannula carefully ensuring it is clear of mucus and any other debris. Take care not to be too firm and avoid using rough/coarse brushes for cleaning as this may damage the tube. After you're done, place it in saline water for at least another five to 10 minutes to soak and become sterile. If you don't have any more saline water, soaking the tube in white vinegar diluted with some water will work also. If you're using disposable plastic tracheal tubes, then skip this step and throw out the tube.
Place the tube back into the tracheostomy hole. Once you've got a cleaned and sterile (or new) tracheal tube in hand, carefully insert it back into the tracheostomy hole whilst holding the neck plate still. Turn the inner tube until it locks back into position securely. You can gently pull the tube forward to make sure that the inner tube has locked into place. This successfully completes your cleaning procedure. Performing this at least two times per day can prevent infections, clogging and other complications.
Cleaning the Stoma
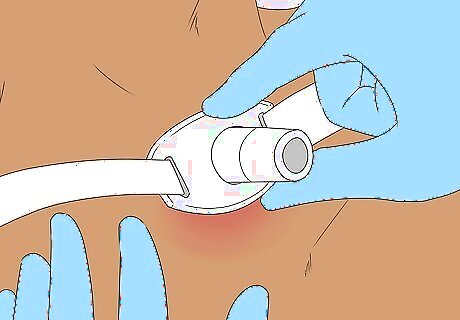
Assess the stoma. The stoma is the hole in the neck/trachea where the tubes are inserted so the patient can breathe. The stoma should be assessed each time after suctioning for skin breakdown and signs of infection. If any symptoms of infection are present (or if anything at all seems questionable), consult a doctor immediately. Symptoms of a stoma infection can include redness, swelling, pain, and the secretion of foul-smelling pus. If a stoma is infected and inflamed, the tracheal tubes will be more difficult to insert. If a stoma is pale or bluish, this may indicate an issue with blood flow to the tissue, and you should contact a doctor right away.

Clean the stoma with an antiseptic. Each time you remove a tracheal tube, clean and disinfect the stoma. Use an antiseptic solution such as betadine solution or something similar. The stoma should be cleaned in a circular motion (with a sterile gauze) starting at the 12 o’clock position and wiping downward to the three o’clock position. Then use a new gauze dipped in antiseptic and wipe towards the nine o’clock position. To clean the lower half of the stoma, wipe with a new gauze from the three o’clock position towards the six o’clock position. Then wipe again from the nine o’clock position moving towards the six o’clock position. Only do this if you've been trained to do so.
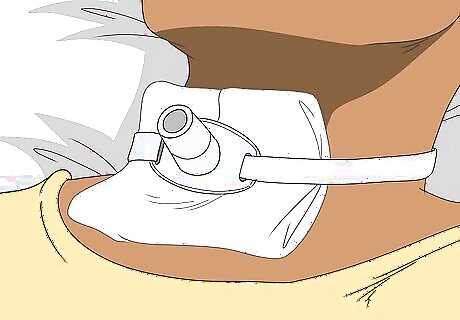
Change the dressing regularly. The dressing around the tracheostomy should be changed at least twice a day. This helps to prevent infection at the stoma site and within the respiratory system (lungs). Changing it also helps to promote the skin's integrity. A new dressing helps to insulate the skin and absorb the secretions that might leak around the stoma. A wet dressing should be changed immediately. This breeds bacteria and can lead to health complications. Don't forget to change the ribbons (ties) that keep the tracheal tube in place if they get soiled or wet. Make sure to hold the tracheal tube in place while changing the ribbons.
Mastering Everyday Care
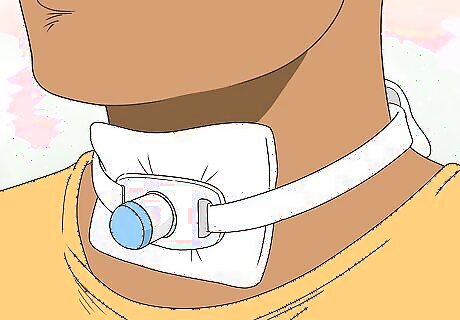
Cover your tube when outside. The reason why doctors and healthcare professionals are so insistent on covering your tracheal tube is that foreign particles and debris can enter an uncovered tube and enter your windpipe. These foreign particles can include dust, sand, and other general pollutants in the atmosphere. This can lead to irritation and even infection, which must be avoided. Entry of debris into your tube leads to excessive mucus production in your windpipe, which can clog up your tube and cause breathing difficulties and infection. Make sure to clean your tracheal tube more often if you spend lots of time outdoors, particularly if it is windy and/or dusty. Talk to your healthcare professional about whether you should cap the tracheostomy tube when you're not using it, or connect it back to a ventilator.
Avoid swimming. Swimming can be very dangerous for any tracheostomy patient. Whilst swimming, the tracheostomy hole is not completely watertight, nor is the cap on the tube. As a result, water entry directly into the tracheostomy hole/tube is quite likely while swimming, which can lead to a condition called “aspiration pneumonia” — water in the lungs that triggers choking. Aspiration pneumonia, even after small amounts of water, can lead to death from choking. The entry of even small amounts of water into the lungs can also increase the risk of a bacterial infection. Cover the tube and also be cautious when taking a bath or shower.
Keep the inhaled air moist. When people breathe in through their nose (and sinuses) the air tends to hold more moisture, which is better for the lungs. However, people with a tracheostomy no longer have this ability, so the air they breathe in is the same humidity as the outside air. In dry climates, this can cause problems, so it's important to try and keep inhaled air as moist as you can. Use a humidifier to help moisten the air during dry conditions at home. Just be sure to clean it regularly so it doesn't develop mold. If you need supplemental oxygen, talk to your physician about whether you should humidify the air.

















Comments
0 comment