views
Identifying Your Insulin Needs
Consult with your doctor to determine the best type of insulin for you. While it’s wise to investigate your options and make an informed medical decision, it’s also important to follow your doctor’s recommendations for how best to manage your blood glucose levels. Talk to your doctor about your concerns and preferences regarding your insulin and let them know if you are interested in changing the type of insulin you currently use. Your first dose of insulin may be based on your weight. Once you begin insulin therapy, you’ll need to follow up with your doctor regularly so they can make adjustments to your dose based on your condition. Your doctor may recommend more than 1 form of insulin, such as a rapid-acting and an intermediate-acting insulin. Your doctor may instruct you to mix these together or take them separately.
Ask about rapid-acting insulin for something that works fast. Rapid-acting insulin reaches the bloodstream 5-15 minutes after you inject it, peaks within 1 hour, and lasts 2-4 hours. Your doctor may suggest keeping some of this on hand in case you need it, such as right before eating a meal. Rapid-acting insulin may also be preferable for use before your evening meal to prevent your blood sugar from getting too low overnight. Some examples of rapid-acting insulin include: Insulin glulisine (Apidra) Insulin aspart (Fiasp and NovoLog) Insulin lispro (Admelog and Humalog) Afrezza (insulin inhaler)

Choose regular or short-acting insulin for multiple daily injections. Regular or short-acting insulin reaches the bloodstream about 15-30 minutes after you inject it, peaks within 2-3 hours, and lasts for 3-6 hours. Your doctor may suggest this as your primary form of insulin and recommend a regular dosing schedule, such as 30 minutes before meals. Some brand names of regular or short-acting insulin include: Humulin R Velosulin R Novolin R
Talk to your doctor about intermediate-acting insulin as a longer-lasting option. Intermediate-acting insulin takes longer to take effect, so it may require a little more planning. It reaches the bloodstream 2-4 hours after you inject it and it peaks within 4-12 hours. This type of insulin also lasts 12-18 hours, so you would not need to give yourself as many injections as you would with regular or short-acting insulin. These can also be used in combination with regular or short-acting insulin if your doctor recommends it. Talk to your doctor to see if this might be a good option for you. Brand names include: Humulin N Novolin N ReliOn
Choose long or ultra long-acting insulin for fewer injections. Opting for a long-acting or even an ultra long-acting insulin may drastically reduce the number of injections that you have to give yourself each day. Take the dose 1 or 2 times daily, depending on your doctor’s recommendation, at the same time(s) every day. If you need to take insulin daily, ask your doctor about switching to one of these types. Don’t mix long-acting insulin with other forms of insulin. Long-acting insulin reaches your bloodstream 4-6 hours after you inject it and it lasts 24 hours or longer. Examples include detemir (Levemir), degludec (Tresiba), and glargine (Basaglar and Lantus). Ultra long-acting insulin takes 1-2 hours to reach your bloodstream and lasts for 24 hours. This is sold under the name glargine u-300 (Toujeo).

Look into pre-mixed insulin if you have vision or dexterity issues. If it’s difficult for you to see the instructions on your insulin label or if you have a hard time drawing up the medication for injections, you may benefit from getting insulin that is pre-mixed. Ask your doctor about pre-mixed insulin for easier injections. An insulin pen or pump can also help to make delivering insulin injections easier if you have vision or dexterity issues. Types of pre-mixed insulin include insulin isophane (Humulin 70/30 or Novolin 70/30), lispro protamine/insulin lispro (Humalog Mix 75/25 or 50/50), and aspart protamine/insulin aspart (NovoLog Mix 70/30). Premixed insulin begins to act 15-30 minutes after you take a dose, and is usually taken 15 minutes before meals. Don’t mix premixed insulin with other types of insulin.

Find out what types of insulin are covered by your insurance. While some types of insulin and insulin delivery methods may be more convenient or preferable, not all of them may be covered by your insurance. Before you choose a medication, call your insurance provider and find out what types of insulin and insulin delivery methods are covered by your insurance and how much of the cost the insurance covers.Tip: Ask your doctor about alternatives to insulin if you have type 2 diabetes. Some people with type 2 diabetes can take medications other than insulin to manage their diabetes, and these medications may be covered by your health insurance if insulin is not.
Using Insulin

Follow your doctor’s instructions for how to administer insulin. If your doctor has prescribed an insulin medication to you, take it exactly as directed. This may include injecting the insulin before each meal during the day, or at other times when your body may require more insulin. Take the exact dose that your doctor recommends, exactly as they have instructed you to.Tip: Ask your doctor if you are unsure about how to use your insulin. You may need to use more than one type of insulin, such as a rapid-acting and a long-acting insulin, and it’s important to deliver these medications exactly as directed by your doctor.
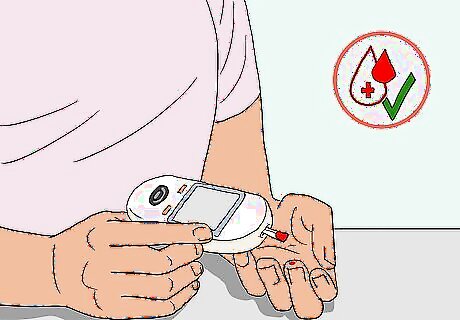
Monitor your blood glucose levels carefully. While using insulin, make sure to test your blood glucose levels on the schedule recommended by your doctor. You may only need to take your blood glucose levels once or twice per day, or you might need to do so more often. Be aware that many factors can impact your blood glucose levels. Some things that may affect your blood glucose levels include your: Food choices Activity level Injection location Timing of insulin injections Health and whether or not you’re sick Stress levels

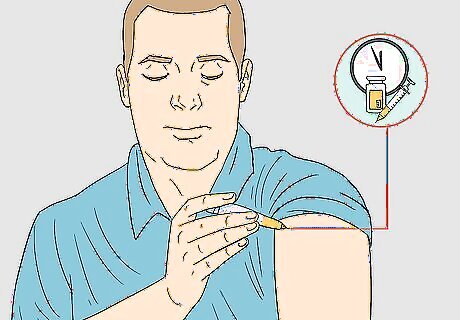
Inject your insulin in the same general area each time. Insulin must be injected into the fat under your skin. This ensures that it will get into your bloodstream. Good locations to use for insulin injections include your buttocks, abdomen, back of your arm, and thigh. The insulin will take effect more quickly or more slowly depending on where you inject it, so it’s important to inject into the same general area each time. Don’t inject into the same exact place every time, but use the same general location for injections. Rotate your injection sites around the same area to avoid hard, fatty deposits. For example, if you deliver your injections into the right side of your abdomen for one dose, inject into the left side the next time.
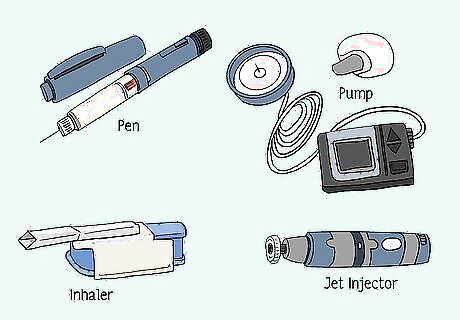
Ask your doctor about devices that make taking insulin easier. The most common way of injecting insulin is with a syringe. However, it can be time-consuming and inconvenient to draw up the medication every time you need it. Ask your doctor about alternatives to syringe injections, such as: Insulin pen. This is a pre-filled device that you can use to dial your desired dose and inject yourself without measuring and mixing your insulin. Using a pen can help you reduce dosing errors. Insulin pump. A small device that delivers a steady stream of insulin 24 hours per day. The insulin is delivered via a small needle that stays put in your skin. You will need to change out the needle about once every week. Insulin pumps mimic the timing of your natural insulin release and can also help you avoid dosing errors. However, they are expensive and require frequent monitoring of your blood glucose levels. Jet injector. This device injects insulin without a needle by using pressure. The insulin is compressed and when you “inject” it, the high-pressure spray allows the insulin to cross your skin and enter your bloodstream. Injectors are also less painful than syringes. Inhaler. This is similar to an asthma inhaler, but it delivers powdered insulin to your lungs, which then gets into your bloodstream.















Comments
0 comment