
views
Cancer affects millions of people across the world and few millions die of it every year. The World Health Organization has warned about an increase in cancer cases by 60 per cent over the next two decades. The biggest increase (an estimated 81 per cent) in new cases will occur in low- and middle-income countries, where survival rates are currently the lowest. Globally, 1 out of 6 people die due to cancer every year. The International Agency for Research on Cancer (IARC) released the updated GLOBOCAN 2020 (global cancer data) on December 14, with new estimates on the global cancer burden, indicating that it has risen to 19.3 million cases and 10 million cancer deaths in 2020.
Common types of cancer in India are cancers of breast, cervix, oral cavity, lung, ovary and colorectal. Cancer doesn’t develop overnight and changes in lifestyle can help us in preventing this life-threatening disease. There are several key steps that can be adopted to reduce the risk of different cancer types as well as screening practices to detect it early.
Eat Healthy, Get Some Exercise
Obesity in adulthood is known to increase the risk of several common types of cancer, such as esophagus, colorectal, breast, endometrium and kidney. Since individual food behaviour and levels of physical activity are determined early in life, promotion of healthy food habits and an active lifestyle need to be started from childhood. Smoking, tobacco consumption, alcohol intake, physical inactivity can increase the risk of cancer. Behavioral modifications, on the other hand, play a key role in preventing it.
Electronic gazettes are making everyone lazy and inactive. Engaging in different physical activities will help in decreasing cancer-related risks. Maintaining a healthy weight might lower the risk of cancer of the breast, prostate, lung, colon and kidney. As a general goal, it is advisable to include at least 30 minutes of physical activity in your daily routine, and it is better if you do more.
Making healthy selections at the grocery store and at mealtime can’t guarantee protection from cancer but it might reduce the risk. Drinking any kind of alcohol can contribute to cancers of the mouth and throat, larynx (voice box), esophagus, colon and rectum, liver and breast. All types of alcoholic drinks, including red and white wine, beer, cocktails, are linked to cancer. Avoid foods with added preservatives, pesticides and other harmful ingredients as a preventive strategy. Eating fewer high-calorie foods and plenty of fruits and vegetables can reduce the risk of cancer.
Check Tobacco Use
Tobacco use is the leading preventable cause of cancer and cancer deaths, contributing to about 1 in 3 cancer deaths annually. While detrimental effects of smoking are well-recognized, the harmful effects of smoking even after diagnosis of cancer are underappreciated. Smoking by cancer patients and survivors causes adverse treatment outcomes, including increased overall mortality, cancer-related mortality, risk of second primary cancer, and considerably increases cancer-treatment toxicity.
There is a clear and unmet need to address tobacco use in cancer patients. The diagnosis of cancer is “the teachable moment”, allowing healthcare professionals the best opportunity to discuss with patients their nicotine addiction and arrive at shared decision-making. An enhanced focus on smoking cessation at the time of cancer diagnosis and active intervention may increase patients’ chances to quit the habit.
Environmental and Occupational Hazards
Environmental factors typically affect the general population through exposures, which are beyond the control of an individual. These factors can be found in the environment as physical (ionizing and non-ionizing radiation, such as exposure to radon or ultraviolet (UV) radiation), chemical (such as asbestos, dioxins and other pollutants found in industrial emissions and second-hand smoke, contaminants or natural constituents found in food and drinking water such as pesticide residues, arsenic or aflatoxins), and biological carcinogens (such as certain viruses).
Exposure to toxic substances, like arsenic, benzene, asbestos, at occupational settings can be dangerous. Occupational health risks are also directly related to physical, chemical and biological factors in the environment. Most common cancers having environmental and occupational determinants are cancers of lung, urinary bladder, skin, larynx, pyriform sinus, nose, and nasal cavity, leukaemia, mesothelioma and angiosarcoma of the liver.
The interventions to reduce exposure to carcinogens and probable carcinogens often lead to reductions in other health risks in the working and living environment. For example, control measures to reduce air pollution from traffic decrease exposure to diesel exhaust gases and, thus, may contribute to the prevention of lung cancer. Establishing linkages between public health programmes for the prevention and control of cancer and programmes and plans of action in the areas of occupational health, environmental health, chemical safety, food safety, etc. will create synergies and help governments, industry, the healthcare sector, NGOs and advocacy groups, and individuals to work together towards the primary prevention of cancer.
Cancers Due to Infection
Infections are one of the leading causes of cancer globally, causing up to 1 in 5 cancer deaths in the developing world. Infection with high-risk types of HPV (Human papillomavirus) causes nearly all cervical cancers. They also cause most anal cancers and many oropharyngeal, vaginal, vulvar, and penile cancers. High-risk HPVs spread easily through direct sexual contact, including vaginal, oral and anal sex.
Helicobacter pylori is a type of bacteria that can cause stomach cancer and a type of lymphoma in the stomach lining. Epstein Barr Virus (EBV) can cause lymphoma and cancers of the nose and throat. EBV is most commonly transmitted by contact with saliva, such as through kissing or by sharing toothbrushes or drinking glasses. It can also be spread by sexual contact, blood transfusions, and organ transplantation.
Chronic infection with Hepatitis B and C virus can cause liver cancer. Both viruses can be transmitted via blood (for example, by sharing needles or through blood transfusions) and from mother to baby at birth. In addition, Hepatitis B virus can also be transmitted via sexual contact. People infected with HIV have increased risks of a number of cancers, especially Kaposi sarcoma, lymphomas (including both non-Hodgkin lymphoma and Hodgkin disease), as well as cancers of the cervix, anus, lung, liver, and throat.
Chemoprevention of Cancer
Using a therapeutic agent to delay or inhibit the progression of the disease is known as chemoprevention and there are many substances, medicines, compounds and agents which are used for chemoprevention of cancer. Tamoxifen and Raloxifene have been found to be useful in reducing the risk of breast cancer by half in asymptomatic breast cancer patients. HPV vaccines are proven to be clinically beneficial to lower the burden of cervical carcinoma.
Diet rich in vitamin C reduces the risk of cervical cancer. Use of agents like celecoxib, Aspirin, non-aspirin NSAIDs, vitamins and minerals for prevention of colorectal cancer is currently under-development. Hormonal therapy along with finasteride has shown positive results in cases of prostate cancer, but side-effects are a matter of concern.
HPV Vaccine Can Help
Most cervical cancers are associated with human papillomavirus or HPV, a sexually transmitted infection. Widespread immunization with the HPV vaccine could reduce the burden of cervical cancer. Gardasil targets two oncogenic (16 and 18) and two nononcogenic (6 and 11) HPV types in quadrivalent vaccine with additional coverage of 31,33,45,52, and 58 in nonavalent vaccine whereas Cervarix targets two oncogenic (16 and 18) HPV types. Gardasil is recommended for males and females aged 9-26 years at 0, 2, 6 month interval while Cervarix is recommended for females aged 9-25 years at 0, 1 and 6 month interval. Children up to the age of 18 years can take only 2 doses at 6-month interval.
Evidence-Based Cancer Prevention and Screening
Prevention and screening of cancer focuses on reducing the cancer incidence and mortality. Prevention of cancer includes change in lifestyle and eating habits, behavioural changes and reduction in environmental and occupational carcinogen exposure, while screening aims at detecting the pre-malignant lesions or cancer at an early stage when chances of cure are much higher.
There is a need for more cancer awareness programmes at frequent intervals with different groups to make people aware about the signs and symptoms of different cancers. Most people are not well-versed with the symptomatology of common cancers, which might help them to reach out for medical assistance at an early stage of the disease.
Signs and symptoms of common cancers in India are:
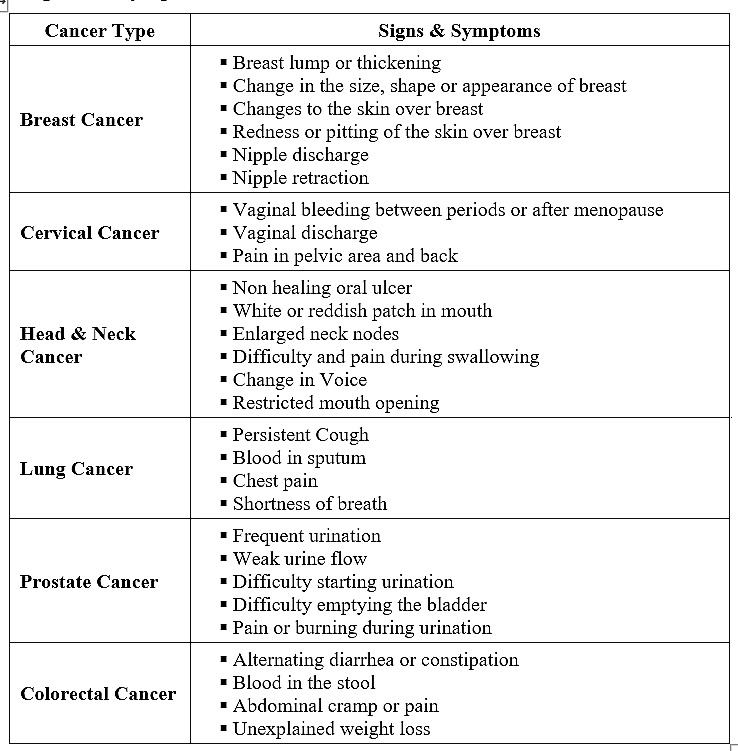
Screening Methods
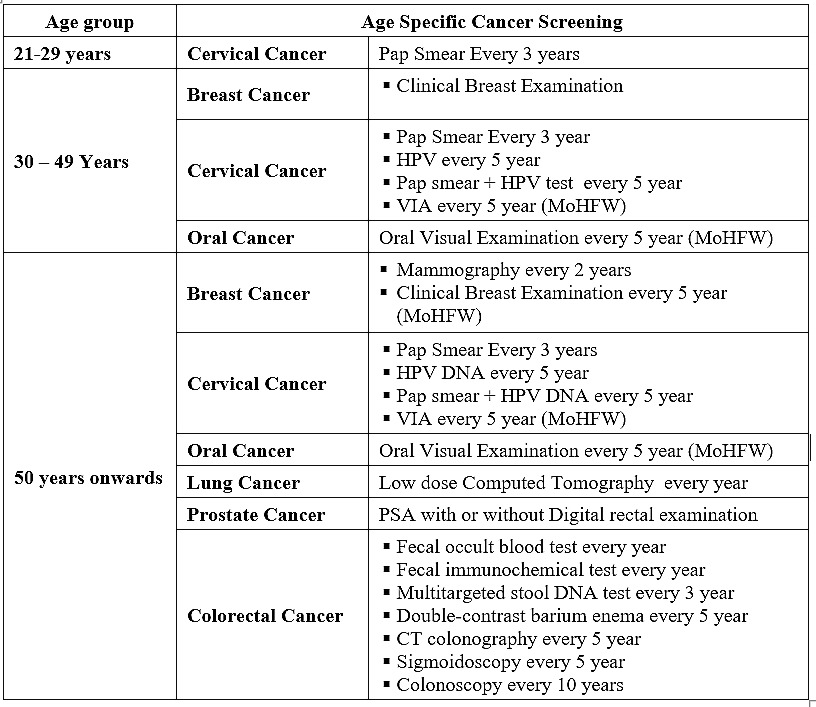
Mammography is most widely recommended as the screening method for breast cancer. Breast self-examination is no more recommended for breast cancer screening as this method failed to decrease mortality due to breast cancer in different studies. Clinical breast examination for breast cancer screening also has limited data. Women aged 21-29 years should be undergo a cervical cytology examination (Pap smear or test) every three years. For women aged 30-65 years, cervical cytology examination must be done every three years and HPV DNA test every five years or Pap test and HPV DNA test every five years. No screening is recommended for women below 21 years.
Currently, lung cancer screening with Low Dose Computed Tomography (LDCT) is recommended every year for individuals aged 50-80 years with smoking history of 20 pack-years, both current and former smokers. Former smoker category includes a person who has quit smoking in the last 15 years. Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that substantially limits life expectancy or is unable or unwilling to undergo curative lung surgery. Prostate cancer screening is recommended for males aged 50 years or above with serum PSA estimation with or without digital rectal examination (DRE).
Colorectal cancer screening is recommended for individuals aged 50-75 years with flexible sigmoidoscopy every five years and colonoscopy every 10 years. Stool based tests i.e. Fecal Immunochemical Test (FIT) and guaiac-based fecal occult blood test (FOBT) are recommended every year. Visual examination of oral cavity can detect premalignant lesions and is a feasible, cost-effective screening method, which can reduce oral cancer-related deaths among high-risk individuals.
Operational framework for management of common cancers in India by the Ministry of Health and Family Welfare recommends Clinical Breast Examination (CBE) for women aged 30-65 years every five years for breast cancer and Visual Inspection with Acetic Acid (VIA) every five years for cervical cancer screening. Oral cancer screening is recommended with Oral Visual Examination every five years for people aged 30-65 years.
Age-wise recommendations for cancer screening:
The Way Ahead
As oncologists have steadily improved their treatment of cancer, their success has evoked calls from various sectors, asking them to get more involved in cancer prevention and screening. Oncologists’ professional organizations and peer group leaders have supported these calls by forming committees and curricula to overcome barriers to involvement in cancer prevention. However, oncologists have been slow to respond to these challenges. Oncologists can play a crucial role in cancer prevention and control by risk assessment of high-risk groups.
Caregivers and family members are keen to know about the cancer and their risk of developing it after diagnosis of cancer among their loved ones. Oncologists have an important role in designing cancer prevention and screening programmes, cancer awareness campaigns, and informing the patients and others about various aspects of cancer and the preventive measures, which includes lifestyle changes, emerging risk factors for cancer and age-specific cancer screening modalities.
Oncology societies and associations have expert members from various oncology specialties along with volunteers and cancer survivors who can educate the public about cancer risks, signs and symptoms, prevention and screening methods. They can also encourage communities to adopt healthy lifestyles, food habits and to go for age-specific cancer screening. These organizations can play leading role in cancer prevention in India where most cases are diagnosed at an advanced stage.
A multipronged strategy is needed to tackle the growing burden of cancer. Lack of nationwide screening guidelines and vaccination strategies are hurdles to reducing the cancer burden.
Theoretically, it should be possible to prevent at least 50 per cent of cancer cases and deaths by applying existing knowledge about the underlying causes of cancer and at least another 10 per cent of cancer deaths by screening. In summary, the unique challenges of preventable cancer burden may be dealt with indigenous and country-specific approaches, which may result in sustainable long-term cancer control.
Dr Abhishek Shankar is Assistant Professor in Department of Radiation Oncology at Lady Hardinge Medical College & SSK Hospital, Delhi; Associate Editor, APJCP; Editor in Chief, APJCC, and Founder Secretary of Indian Society of Clinical Oncology. He tweets with @ShankarAbhishek. Dr Deepak Saini is Project Officer at Cancer Control and Prevention Division of Indian Society of Clinical Oncology, Delhi. Views are personal.
Read all the Latest News, Breaking News and Coronavirus News here














Comments
0 comment