views
It is often said that time is relative. Indeed so, if one looks at it from the perspective of the last two months, which have been like falling into a dark bottomless pit of despair, agony, crisis, mayhem and death, when the nation was being ravaged by the second wave of COVID-19. News of despondency almost made the entire nation numb to the extent that emotions stopped working beyond a point. To hear of or witness death, and of young children getting orphaned, perhaps became a regular affair.
Even though it is true that the absolute number of cases have been steadily coming down and that the logistical issues associated with transport of oxygen have been considerably addressed by the central government and for which it deserves credit, yet apprehensions and fear of an impending third wave remain palpable. It is also true that despite present shortage, it is only a matter of time before the vaccine issue gets sorted out too, and supply would more than match the demand in the coming months, with certain estimates anticipating over 1.7 billion doses becoming available in the next six months. The decision of the Narendra Modi government to procure 75 per cent of the vaccines and supply them to states has been a welcome step in the fight against the pandemic. But the battle is far from over.
Nevertheless, the following are a key set of policy reforms that India must initiate to remain better prepared for future pandemics or any national health crisis like the one it is facing now.
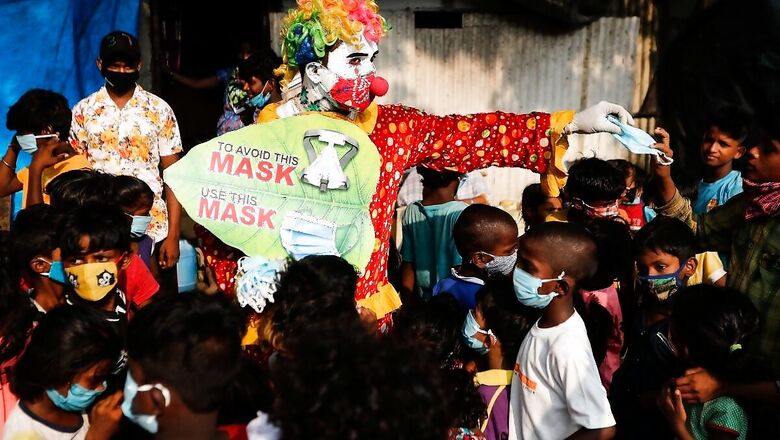
Make Wearing of Mask in Public Places Legally Enforceable
It is rather sad and appalling that in spite of the apocalypse India is facing due to COVID 2.0, the country is yet to get its act together in terms of making wearing of masks in public places a legally enforceable activity. Shockingly, as per Union government’s own admission, around 50 per cent people still do not wear masks. COVID-19 may be life threatening but it cannot walk or fly on its own unless COVID-imbibed droplets that emanate from mouth of a carrier host get a chance to either float in the air or reach directly the mouth or nose of a potential victim.
Therefore, no amount of preparation for future pandemics would be of any use unless India can inculcate some civic sense among the masses, either by education or by the fear of the cane or prosecution. Sadly, here neither happens. Even the most rudimentary action by policemen on violators is deemed severe transgression of human rights and needless furore is created. India already has the Epidemic Diseases Act in place and it is not impossible to make proper wearing of mask (covering both nose and mouth instead of the chin) legally mandatory within its purview.
Junk Cheap Populism, Invest in Healthcare Infra
No country’s government has unlimited money for unlimited expenditure on all kinds of freebies along with investments in infrastructure. It can do either of the two. Therefore, time has come for India to seriously contemplate as to whether it should continue with its vote bank-driven populism policies, or instead, spend the precious money on development of infrastructure, especially in the realm of healthcare. There would be resistance against it, but there is no reason why rich and upper middle class should continue to get hefty subsidies on domestic electricity supply for using expensive gadgets. The same goes for water and even rail fare.
The culture of charging less than cost of production and not raising prices must end. There is no reason why long-distance fares of express trains should be subsidised. It is time to allow competition in electricity market, which would automatically reduce prices and bring in efficiency. Every penny wasted on subsidising such stuff is a missed opportunity to invest more in healthcare infrastructure among others. Subsidies, if at all, should be directed towards start-up ventures and not on consumptions that people can easily pay for.
In fact, Delhi is a classic example of how to waste precious revenue on cheap and petty populistic subsidies for urban rich and middle class, and eventually, in spite of being one of the richest city-states of India, stare at a shocking healthcare crisis because it simply did not spend enough on expanding its healthcare infrastructure that would have been commensurate with its growing population. In fact, no state of India gets so much of institutional support from the central government as the city-state of Delhi, and yet it faltered miserably during COVID 2.0 because of misplaced priorities and focus on cheap populism to win votes. Likewise, poll-time populistic promises of some political parties to shower voters with freebies of TV sets and other consumer durables must also end.
India Needs National Healthcare Services Regulatory Authority
Much on the lines of the Telecom Regulatory Authority of India (TRAI) and the Insurance Regulatory Authority of India (IRDA), India may now need a National Healthcare Services Regulatory Authority. While the medical fraternity deserves the nation’s unfettered gratitude for their services during the pandemic, it is also true that several unscrupulous elements have been taking advantage of the pandemic situation. There has also been news of rampant black marketing of critical drugs, artificial shortage of the same created by market manipulators, and considerable discrepancies in the cost of COVID treatment among hospitals. Some select nursing homes have been severely criticised for massively inflated amounts charged for COVID treatment.
Therefore, for bringing uniformity in quality and cost of service delivery, India may need to create a regulatory environment for the entire healthcare sector including super-specialty hospitals and nursing homes. Price band must be set for cost of treatment.
India Needs More Doctors, Paramedics & Hospitals
As per a Government of India submission in the Lok Sabha last year, India has 541 medical colleges with a cumulative seat count of 80,312 for intakes. The submission further stated that Government of India was working on setting up 157 additional medical colleges of which 43 are already functional. While this is commendable, India also needs to relax its regulatory norms to allow low-cost or budget hospitals to emerge across the spectrum of rural and suburban India.
There is absolutely no reason why innovation for budget hospitals cannot be implemented if the same can be done in the realm of other sectors. Also, there is a need for drastic restructuring of undergraduate courses whereby mainstream colleges must be encouraged to inculcate more of paramedical courses. The pandemic vindicated how much India needs a vast army of paramedical professionals.
Further, apart from training more undergraduates in such vocations, what can also be done is to permit paramedic personnel like pharmacists, radiographers and laboratory technicians to supplement as nursing assistants during a pandemic-related emergency situation by reskilling them with basic know-how of administering drugs and injections, reading vital parameters and maintaining basic database of patients. This can drastically augment the workforce of patient-care personnel as and when needed.
Bring Department of Biotechnology under PMO
Much on the lines of Department of Atomic Energy and Department of Space, perhaps the time has come to give equal importance to Department of Biotechnology and allow it to be run entirely by technocrats. India needs to emulate its success in software sector, in the realm of biotechnology as well, given the emerging threats from pandemics or apparent bio warfare scenario that the world is witnessing, and the enormity of havoc that they have demonstrated to wreak.
India not just needs to enhance its proficiency in predicting future pandemics, but also needs to create a vibrant ecosystem for biotech start-ups and follow the template of its success in IT services industry to become a global leader in biotechnology as well as become a critical player in the global biotech supply chain. While India already has proficiency in making generic medicines and vaccines at global scale, it needs to scale up and become a frontrunner in innovative countering of pathogenic threats. For that to happen, an ideal ecosystem that brings together start-ups, biotechnology or microbiology departments of universities, industry and government institutions to counter future non-conventional threats emerging from microbes is needed.
Better Pay and Training for ASHA Workers
During the pandemic, the ASHA workers played a critical role in creating awareness in rural India as also in allaying fake apprehensions regarding vaccines. ASHA workers literally became eyes and ears of the governments regarding the situation in rural India, which got badly hit during the second wave. Given the inadequacy of healthcare professionals in rural India, the function of ASHA workers needs to be institutionalised with regularised salaries and specialised training in addition to creating more opportunities for induction of more qualified rural women as ASHA Assistants.
Strategic Reserve of Critical Medicines
Much on the lines of strategic reserves of crude oil and foodgrains, there is perhaps a pertinent need now for the country to have a strategic reserve of critical medicines and medical devices. The pandemic showed how it can create global supply chain disruptions for critical medicines, their raw materials and also how the new-age pandemics have the potential to skyrocket the demand for certain medicines abruptly. It is from this perspective, perhaps, that India needs to deliberate on the necessity of having a reserve stock of a broad spectrum of critical medicines. Given the fact that India is one of the largest manufacturers of generic drugs in the world, and given its proficiency in industrial scale manufacturing, it would not be difficult for India to stockpile such medicines as well as devices like ventilators or oxygen concentrators.
Lateral Entry of Healthcare Professionals in Health Ministry a Must
Global scale pandemics are not like any other generic crisis. From anticipating a pandemic-induced crisis to managing the same and recuperating a nation post- pandemic, one requires a very specific set of skills that is essentially different from what a bureaucrat or a technocrat or even a general physician dealing with patients have. The generic way of functioning of health ministries, be it in the state or at the central level, need to be radically restructured.
Across the world, the pandemic vindicated how pre-emptive planning and anticipation of crisis can play a critical role in managing the pandemic better. Therefore, India needs more lateral entry of health professionals, biotech experts and scientists in health ministries, at state and central level. They can genuinely complement the work of the policymakers and officials.
Reactivate Telemedicine on Mission Mode
While the medical fraternity across India has worked tirelessly to confront the pandemic with all their valour, there are still plausible gaps so far as rural healthcare is concerned. It is thus time to reactivate the telemedicine revolution once again in India. India’s nearly 5.5 lakh gram panchayats are gradually getting connected with Wi-Fi through a Government of India project. This creates the perfect opportunity for making every panchayat office a Telemedicine Interactive Centre (TIC) for village-level awareness programmes during health crisis situations.
The pandemic showed that nearly 85 per cent of COVID-infected patients did not need hospitalisation and could be treated at home with proper medical guidance. The combination of telemedicine centres at panchayat offices along with ASHA workers armed with smart devices to connect patients with doctors can play a key role in bridging gaps and reducing rural mortalities. Also, with India already witnessing a digital boom and with smartphones being no more a rarity in rural India, a bunch of doctors sitting in a state capital or district headquarters can adequately take care of thousands of villagers without physical visits by piggybacking on the digital revolution India has been witnessing for years now.
Revamp Primary Health Centres with PPP Model
India not only needs restructuring of district hospitals but also a major revamp of the rural primary health centres. In this respect, the ideal way to go forward would be to forge partnerships with India-based foundations and charitable organisations that run hospitals or institutions, and gradually allow them to take over part of the operations. The likes of Ramakrishna Mission Seva Pratishthan, Bharat Sevashram Sangha, Christian Medical College of Vellore and also the likes of the Tata Trust, Reliance Foundation, Azim Premji Foundation to name a few can be roped in for managing primary health centres and thoroughly revamp them as modern clinics.
This may play a key role in augmenting the basic efficacy of rural primary health centres, may attract more talent from medical fraternity and can reduce the dependence of rural citizens on city-based hospitals. India’s next generation healthcare modernisation has to be rural-centric and there is no better way to go forward than to forge alliance between government health departments and private NGOs.
Time to Consider Population Control
By June 5, 2021, it was reported that India had already administered a greater number of people (17.2 crore) with the first dose of COVID vaccine than the US, which had by then administered first dose to 16.9 crore people. However, when compared as percentage of population, the US had administered first dose to nearly 50 per cent of its total population of around 33 crore, whereas for India, the figures would less than 13 per cent considering India’s total population at an estimated 135 crore.
The difference, therefore, lies in the quantum of population and for India, given the enormity of its population, the challenges of vaccinating the entire eligible population or managing a pandemic is always humongous. No country can manage it seamlessly. It is, therefore, high time that the Government of India seriously considers drafting laws for controlling the population growth rates. If the Indian population keeps growing at the current rate and reaches 150-crore mark in the next 10 years and if in a decade’s time the world faces a similar health crisis, then however much India prepares, it would always be an uphill task to manage the situation unless something is done to check population growth rate.
Fight Disinformation on Mission Mode
Sadly, for more than a year now, since COVID-19 arrived in India, the country is not only confronting the pandemic but also a series of disinformation campaign by vested interests and certain political personalities that often created suspicions in the minds of people and derailed the efforts of the institutions combating the pandemic. Vested political interests left no stone unturned to create confusion and apprehensions about Indian-made vaccines. Some even most ridiculously termed it as ‘BJP’s Vaccine’ and exhorted their supporters not to take it.
Misinformation was also spread about the side-effects of COVID vaccines that created needless fear among the rural masses in certain states. In a pandemic situation, where the masses are already in panic mode, strict action is needed to curb all kinds of disinformation campaigns and their amplification by social media platforms. The government must create a template to invoke strict penalties and prosecute those looking for opportunities to create chaos and disruption during the nation’s combat against any global-scale pandemic akin to a national crisis.
The Age of Biowarfare is Back: Be Prepared
Even as the world continues to face the pandemic crisis, the tell-tale suspicions surrounding the lab origin of COVID-19 and that the virus was deliberately tweaked to make it more infectious in a laboratory in Wuhan, China, has been gaining ground. In reality, no one can deny that the single biggest beneficiary of the political, economic and social crisis wreaked by COVID-19 has been China, which has seen its industrial wheels churning like never before even as the world has been brought down to a standstill by the virus and subsequent lockdowns. The question that, therefore, arises is this: Is the world merely facing a pandemic or a biological war under the veil of a pandemic? The chances of the latter seem more plausible with each passing day.
Therefore, it is perhaps time for India to consider creating a security architecture to counter bio warfare threats with as much gravity as conventional and nuclear threats. India has thousands of institutions, laboratories, research centres, university departments, pharma and biotechnology companies who work in the realm of both fundamentals of molecular biology as well as applied biotechnology and formulations. However, biological security or security from bio warfare or defending nation from weaponised viruses as discourses have never gained much traction in India. Now is the time.
There is an urgent need for greater civil-military fusion to strive for 360-degree security of the country including from bio warfare threats. The COVID pandemic has provided enough reasons to wonder how future warfare might be shaped, where the perpetrator may debilitate nation after nation without firing a single shot or calling out war. In such a scenario, it may not be combat jets and or submarines but a readymade arsenal of vaccines, and much on the lines of a nuclear deterrent, perhaps an arsenal of laboratory made bio warfare agents of one’s own, acting as deterrents, which can prevent the perpetrator from unleashing havoc in future once again.
Read all the Latest News, Breaking News and Coronavirus News here.














Comments
0 comment