
views
Measuring Blood Pressure Lying Down
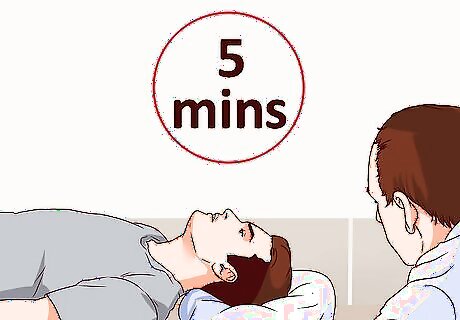
Ask the person to lie down for five minutes. He should be completely flat on a table, bed or couch. Wrap the sphygmomanometer, or blood pressure gauge, armband firmly around the person’s upper right arm and secure it with the Velcro strip.
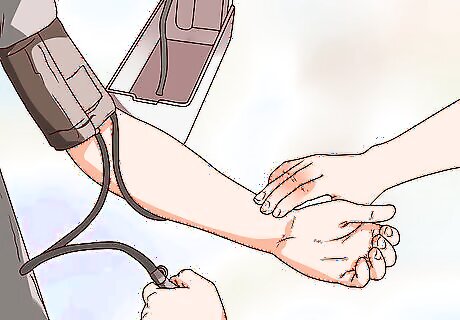
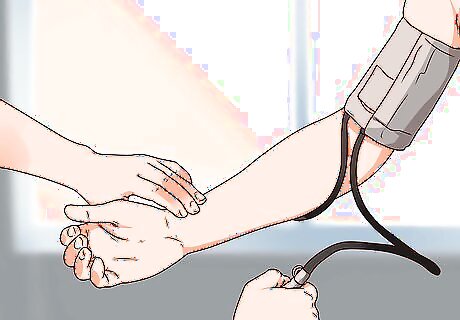
Place your stethoscope over the brachial artery. With the blood pressure cuff wrapped around the person's arm, have her palm facing upwards and place the stethoscope on the inside of the elbow. The stethoscope has a large surface area, so placing it on the inside surface of the elbow should ensure that it covers the brachial artery, which travels through that area. You will be listening to sounds in the brachial artery as your way to measure blood pressure.
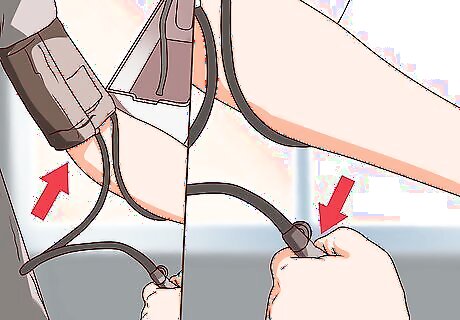
Inflate the armband with the pump. Generally you should inflate it to around 200 as your starting number, and gradually deflate it from there. As the cuff deflates, look for the systolic blood pressure reading. Systolic blood pressure is the force of the blood pumping through the arteries, and it is usually between 110 and 140. You will recognize the reading for the systolic blood pressure at the moment you begin to hear the "thump" sounds in your stethoscope. This is the sound of blood flowing through the brachial artery. Keep note of this number in your head as you continue listening while the cuff deflates.
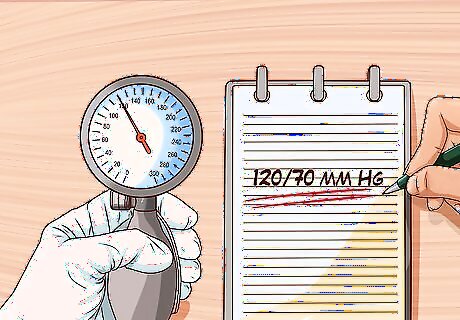
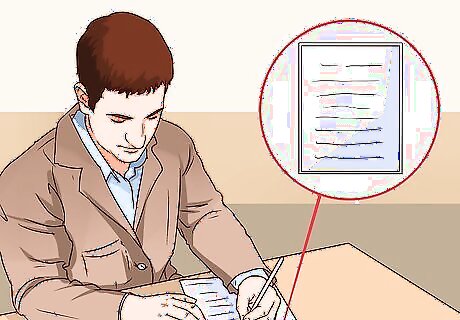
Record the diastolic reading after the sound clears. This number should be lower, usually between 60 and 90. It is the pressure on the arteries between heartbeats. Write the systolic blood pressure number, a slash, and then the diastolic blood pressure number. Both are measured in millimeters of mercury, or mm Hg. For example, you might write “120/70 mm Hg.”

Finish by taking the radial pulse reading. This is the pulse you find by placing your index and middle finger over the inside right wrist. When you feel the patient’s pulse, watch your clock or watch for exactly 60 seconds and count the beats. Most people have a pulse between 60 and 100 beats per minute (BPM). If the patient’s pulse is above this, he may not be able to stand and continue the test. Write down the pulse (or heart rate), and then prepare yourself for the next portions of the test where you will ask the person to stand.
Measuring Blood Pressure Standing Up
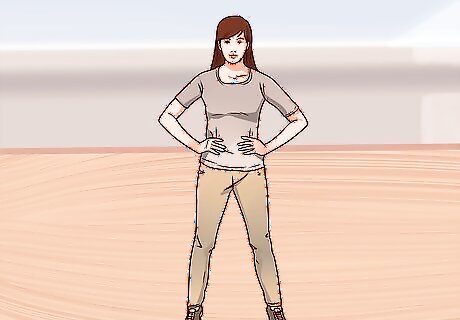
Ask the person to stand. Ensure that she has support to lean on if she is unstable on her feet. Ask them to hold on to something with her left arm so that you can take blood pressure and pulse on the right arm. Wait until the patient is stable, but you must take the tests as soon as possible (within the first minute) after standing. Inform the person that if she is feeling lightheaded or faint at any point she should let you know, so that you can sit her down. Although she needs to be standing in order for the test to be successfully performed, you do not want to do this at the expense of them passing out.
Pump up the arm band again. Take a systolic and diastolic blood pressure reading, and record both of these values. Also repeat the pulse test and write down your results.
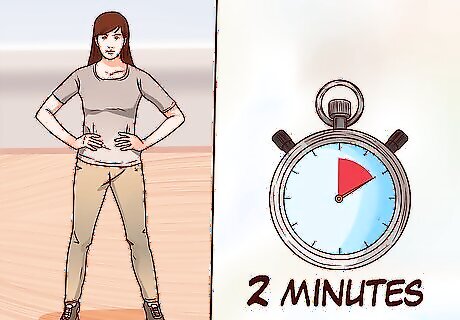
Wait two minutes. The patient should continue to stand. Two minutes after the first standing measurement (and after three minutes total of standing), a second standing blood pressure value should be obtained. Inflate the cuff again and record the systolic and diastolic blood pressures. In normal physiology, the person's systolic and diastolic readings should be higher in the second standing reading than they were in the first, as the body has had more time to compensate for the change in posture.
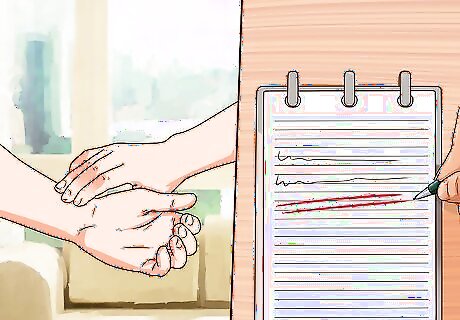
Take one last measurement of the patient’s pulse (measure at the wrist). Write down your findings. Ask the person to sit back down as you calculate blood pressure changes and look over the results.
Evaluating Results
Evaluate the results. Subtract the standing (1 minute) values from the laying down readings. Also subtract the standing (3 minute) values from the laying down values, for a comparison and to see how quickly the body adapts. Judge whether the person is likely to be suffering from orthostatic hypotension. If the systolic pressure decreases by 20 mm Hg or if the diastolic pressure decreases by 10 mm Hg, they likely have this condition. Note that the condition is diagnosed based on the 1 minute standing blood pressure, not the 3 minute one (the 3 minute one simply provides a comparison to see how quickly the body adapts when given more time to stand). Also consider whether the patient’s pulse increases by a normal rate. It is usual for the pulse to increase by 10 to 15 beats per minute. However, if the beats increase by 20 beats per minute or more, she should see a doctor for further evaluation.

Consider the person's symptoms. Regardless of the difference between the blood pressure values lying down and standing, if the person feels lightheaded and/or dizzy consistently upon standing he needs to be seen by a doctor for a professional evaluation of what may be causing these symptoms. The diagnosis of "orthostatic hypotension" can be based on these symptoms alone, regardless of the difference in numerical blood pressure values, so it is important to ask the person about any symptoms he may be experiencing when he suddenly stands.

Understand why it is important to measure orthostatic blood pressure. Having "orthostatic hypotension" (low blood pressure immediately upon standing) is very common, particularly among the elderly. It leads to symptoms such as light-headedness and/or dizziness upon standing, and it poses the risk of someone passing out when she stands up due to insufficient blood flow. It is important to be aware of "orthostatic hypotension" in order to correct or improve it as best as possible. In the elderly, common causes of orthostatic hypotension include medications the person is taking, dehydration, insufficient salt consumption (although too much salt can lead to overly elevated blood pressure), or simply a delayed response of the blood pressure after standing, which, to some degree, correlates with the natural aging process. Orthostatic hypotension is far less common in young people. However, it can sometimes occur as the result of other diseases (Parkinson's disease, paraneoplastic syndromes, etc.), extreme dehydration, or large amounts of blood loss secondary to trauma.

















Comments
0 comment