views
Taking Methotrexate Orally
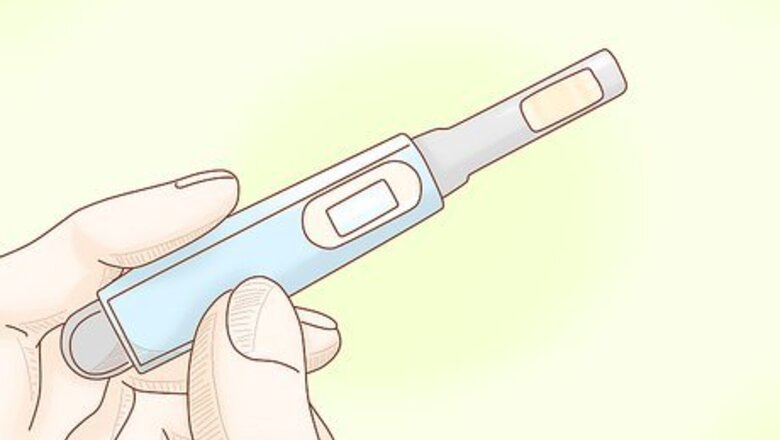
Take a pregnancy test first if you are sexually active. If there’s a chance you may be pregnant, it’s important to take a pregnancy test before starting methotrexate. This medication can cause severe birth defects or miscarriage if you take it while you’re pregnant. If you’re sexually active, talk to your doctor about using a hormonal birth control method (such as “the pill”) before you start taking methotrexate.
Get a blood test before taking methotrexate. Your doctor will likely want to check your kidney and liver functioning to make sure methotrexate is right for you. They’ll also look at your blood cell counts to monitor your immune system and overall health. The results will help them determine your proper starting dosage. Your doctor will probably have you come in for regular blood tests to monitor any changes or abnormalities. Starting out, expect to have a blood test every 2 weeks for the first month or so (particularly if you have cancer). If there’s any chance you may have been exposed to tuberculosis, ask your doctor about getting a PPD skin test. This test can check for a latent TB infection, which could become active if you start taking methotrexate or another medication that suppresses your immune system.

Take your prescribed dosage on the same day once per week. Your dosage depends on your body weight and the condition you’re treating. If you have cancer, your doctor will probably start you off taking 10 to 30 mg once per day or 5 to 50 mg once per week. For psoriasis, you may be prescribed 10 to 25 mg once per week. The typical dosage for rheumatoid arthritis is 7.5 mg once per week. It’s critical to take this medication exactly as prescribed. Taking the wrong dose can cause dangerous side effects, such as a severely reduced blood cell count. Double check with your doctor or pharmacist to make sure you understand your dosage correctly, and always ask if you have any questions or uncertainty about how much to take and how often. This medication is usually taken once a week. Choose 1 day a week to take your pills and stick to that schedule unless your doctor tells you to do otherwise. If you miss a dose, you can safely take it the next day. If it has been over 2 days since you missed your dose, wait until your next weekly scheduled dose. Store the pills in a medicine cabinet that children do not have access to. Check in with your doctor on a regular basis so they can monitor the effects and adjust your dosage accordingly.
Take half of your dose at a time (on the same day) to ease side effects. If you have severe side effects, ask your doctor or pharmacist if it’s okay to split your pills and spread out the dosage throughout the day. Some people find it helpful to take half of their pills in the morning of their dosing day and the other half about 12 hours later. However you split it up, always take it with food to prevent uncomfortable side effects. Talk to your doctor about splitting your dose before you try it on your own. Swallow the pills with 8 fluid ounces (240 mL) of water.
Injecting Methotrexate
Schedule one day per week for your injection. Methotrexate can be injected by you, a friend, or family member once a week. Pick a day that works for you and stick to it. You can inject it at home or in any private place where you feel comfortable. Don’t try to inject yourself while on public transit (riding the bus, subway, or on a plane) because any turbulence will encumber your ability to insert the needle properly. Set up a regular time with a friend or family member to administer your injection. Mark your calendar ahead of time or set an alarm on your phone so you don’t forget. Choose a place that is free of distractions (like activity from pets or children).
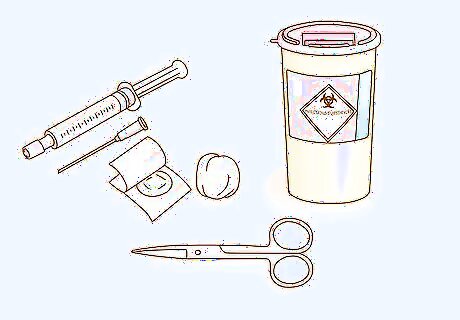
Get all of your equipment ready before your injection. Your prescribed kit will come with 1 pre-filled syringe, 1 needle, 1 cytotoxic sharps bin, 1 cotton ball, 1 dot plaster, and 1 pair of scissors. Store your prefilled syringes at room temperature (68 to 77 °F (20 to 25 °C)) in a place that children do not have access to (like a high-set medicine cabinet). Some syringes need to be stored in the refrigerator, so ask your doctor or check the pamphlet that came with your kit. You can leave the syringes that require refrigeration out of the fridge for up to 30 minutes before injecting. Some kits come with alcohol pads, but if not, you can easily get them from your local drugstore or pharmacy. You may also want to have a clean paper towel handy to lay out your materials on a clean surface.

Wash your hands thoroughly with antibacterial soap. Your hands need to be clean of any bacteria, dirt, or debris to prevent contamination. Dry your hands well with a clean cloth or paper towel. Lather your hands for at least 20 seconds with soap before rinsing them off under warm water. Avoid using hand sanitizer in lieu of washing your hands—these don’t kill all forms of bacteria that could contaminate the materials or the injection site.
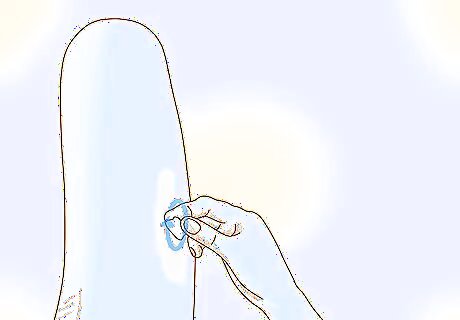
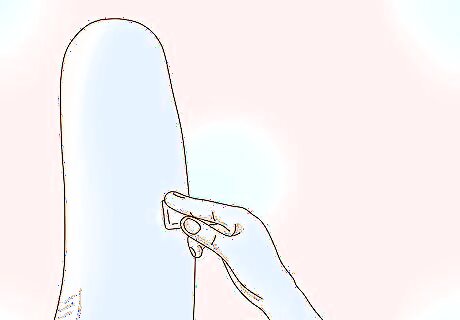
Choose an injection site and wipe it with an alcohol swab. Methotrexate should be injected into your thigh or stomach area and you should change the injection site each week. Pick an area where you can pinch 1 inch (2.5 cm) of fat (like your outer upper thigh or below your navel). Don’t inject it into your arms, within 2 inches (5.1 cm) of your navel, or into other areas of your body. Once you’ve chosen your injection site, wipe the area with an alcohol swab and let it dry naturally (don’t blow or fan it dry). Alternate between injecting on your left and right side every week to prevent soreness. Avoid injecting into skin that’s tender, bruised, red, or scaly, or in areas with scars or stretch marks. Don’t touch the area again before injecting the drug.
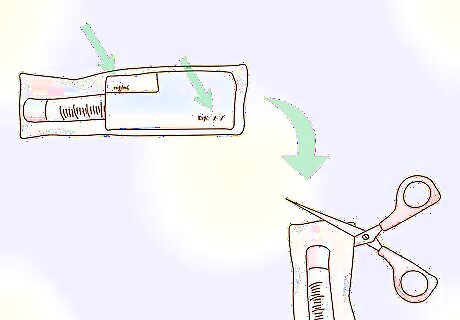
Check the package for your name, the expiration date, and the correct dosage. Even if you’ve just received the kit, it’s important to make sure that you’ve received the right prescription and that it’s not expired. Once you’ve confirmed these facts, use scissors to cut the top of the sealed bag containing the syringe. Handle the bag and syringe with care—don’t try to tear the bag open with your teeth or any other sharp object. Check the liquid inside the syringe—it should be clear and yellow. If you see any particles or cloudiness, don’t inject it and call your doctor or pharmacist right away. If the expiration date has passed or if you notice the bag has been broken or damaged, do not use that syringe and call your doctor or pharmacist immediately.
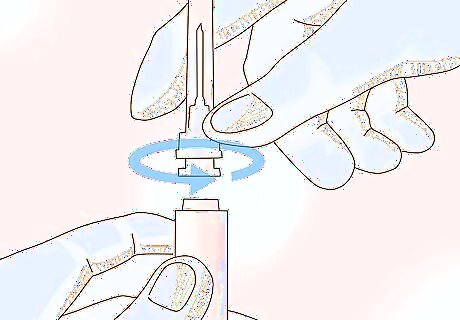
Attach the needle to the syringe. Loosen the needle cover (but don’t remove it) and insert it into the end of the syringe with the sharp point facing out. Don’t let anything touch the needle once the cover is removed. If you accidentally brush it against your clothing or set it down on an unclean surface, discard it into the sharps box and insert a new needle. If the syringe has a safety stopper that keeps the plunger from going down into the barrel, remove it. Don’t let anyone handle the syringe unless they’ve washed their hands as well. To prevent infections, use a new, clean needle every time you take an injection.
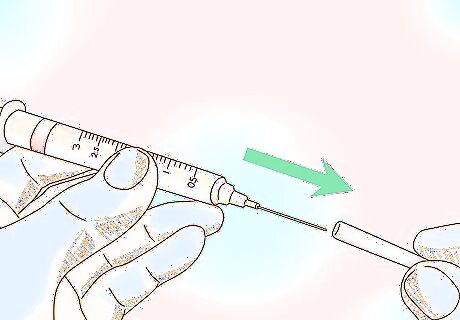
Hold the syringe like a pen and remove the needle cover. Grip the syringe down low on the barrel as if you’re going to write your name with it. Avoid holding it too loose or too tight so you don’t drop it. With your other clean hand, carefully remove the needle cover and set it aside. You might see a drop of liquid at the end of the needle—don’t worry, that’s normal.
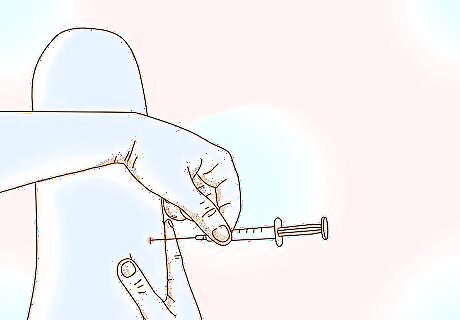
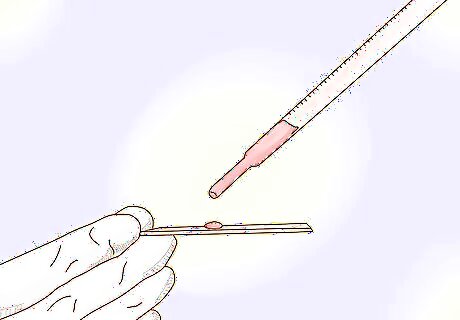
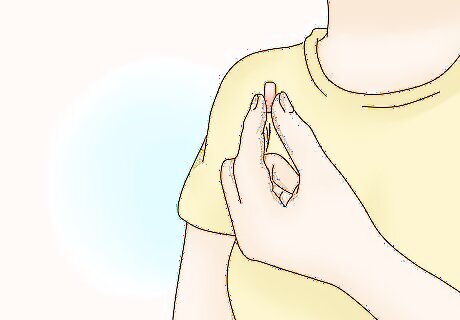
Pinch the skin at the injection site and insert the needle at a 45° angle. Pinching the skin will prevent the injection from going into your muscle. Use a dart-like motion to quickly insert the needle into your skin at a 45° angle (a perfect diagonal). Have a clean cotton ball or gauze pad ready for after the injection.
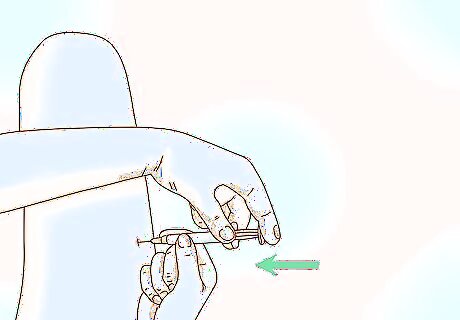
Push the plunger all the way down and remove it at the same angle. Once the needle is in place, use your index and middle fingers to slowly push the plunger down until all of the liquid is injected. Be sure to hold both of your hands steady while you push the plunger in. Then pull the needle out of your skin at the same 45° angle. Make sure the syringe is completely empty before removing the needle.
Apply pressure to the injection site with a cotton ball. Pressing a cotton ball or gauze pad onto the injection site will help stop the bleeding faster and shield the small opening from bacteria. Press it for about 10 seconds. Don’t rub the area because this can irritate your skin. If the small opening is still bleeding after pressing it, cover it with a clean bandage.
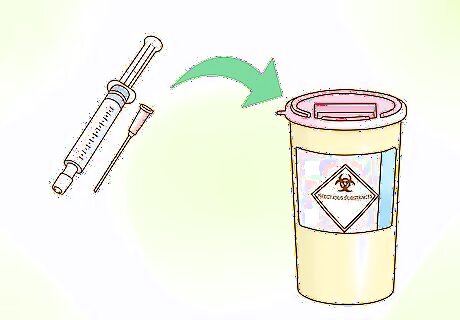
Discard the used syringe and needle into the sharps disposal container. Don’t touch the used needle afterward and discard it into the disposal container right away. Used needles and syringes are biohazardous, so don’t toss any of these materials into your trash. When your container is full, check your state’s sharps disposal regulations at http://www.fda.gov/safesharpsdisposal. If you don’t have a sharps disposal container, you can use a heavy-duty plastic container with a tight-fitting, puncture-resistant lid. Make sure it’s leak-proof and is able to sit upright. Make a label for it that says “hazardous waste” or “biohazardous materials” to keep people from tampering with it. The syringe package, cotton ball, and alcohol pads can be tossed in your regular trash.
Managing Side Effects
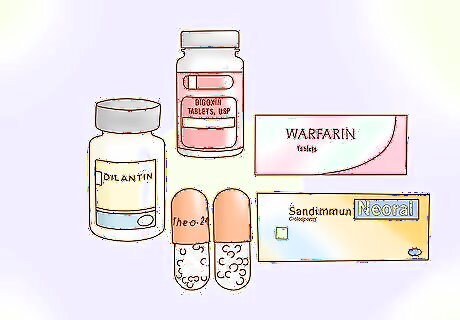
Avoid taking drugs that interfere with methotrexate. Avoid phenytoin (Dilantin), theophylline (Theo-24), digoxin (Digox), ciclosporin (Sandimmune), warfarin (Jantoven), and certain antibiotics (such as penicillins, glycopeptides, ciprofloxacin, cefalotin, sulfonamides, trimethoprim/sulfamethoxazole, tetracycline, and chloramphenicol) when you’re taking methotrexate. If you’ve been prescribed these drugs for other conditions, talk to your doctor about alternatives that won’t interfere with your treatment. Acitretin (Soriatane), azathioprine (Imuran), isotretinoin (Accutane), sulfasalazine (Azulfidine), or tretinoin (Vesanoid) are other drugs to avoid when taking methotrexate.
Take methotrexate with food or after eating to ease an upset stomach. Nausea, vomiting, and diarrhea are common side effects of methotrexate. Taking your medication with food or after a meal will help ease these effects. If you develop severe nausea, vomiting, or diarrhea, talk to your doctor as soon as possible to figure out a solution. Avoid highly seasoned foods (like curries and sauces) and opt for milder foods like oats, yogurt, bread, avocado, and lightly-seasoned vegetables and proteins.

Take a folic acid supplement 24 hours after to help manage any side effects. Methotrexate depletes your body of folate, causing nausea, vomiting, headaches, dizziness, and fatigue. Less common side effects include mouth ulcers and hair loss. Your doctor may recommend that you take 1 mg to 5 mg of folic acid once per week. Taking it a day after you take methotrexate is best, but you can take it at the same time or any time you feel side effects coming on.

Avoid alcohol to reduce the risk of developing liver cirrhosis. Methotrexate is hard on your liver, especially if you take it over a long period of time. Symptoms of liver damage include pain in the upper right part of your stomach, jaundice (yellowing of the skin and/or eyes), and/or flu-like symptoms. Call your doctor immediately if you suspect your liver might be damaged. If you are elderly, obese, or diabetic, you have a higher risk of liver damage. If you’ve ever had alcoholism or liver disease, talk to your doctor about alternative medications.

Avoid hard, acidic, and spicy foods to prevent or help heal mouth ulcers. Eating crunchy, acidic, or spicy foods can irritate your mouth and make existing ulcers worse. That means chips, crackers, pretzels, citrus fruits, alcohol, hot sauce, and spicy peppers are off the table for the time being. Cut your food into small pieces and choose soft foods like potatoes, well-cooked vegetables, soups, and breads. Do a saltwater rinse or swish with mouthwash that has lidocaine to help heal ulcers and treat the pain.
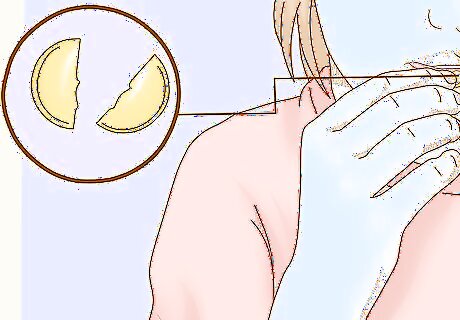
Avoid unnecessary exposure to UV light. Methotrexate can make your skin more sensitive to sunlight, especially if you are taking it for psoriasis. So, avoid tanning beds, UV lamps, or prolonged exposure to sunlight. If you go outside on a sunny day, protect your skin with sunscreen, clothing, and sunglasses. Apply a quarter-sized amount of SPF 30 (and up) sunscreen to each exposed section of your body about 15 minutes before sun exposure.



















Comments
0 comment