
views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
Educating Your Child

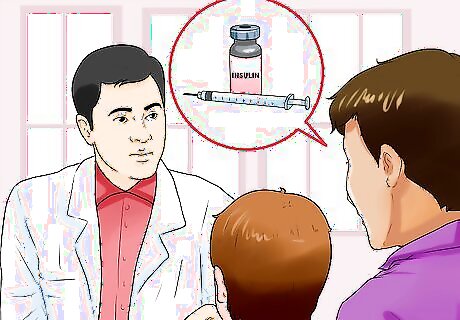
Assemble a team of professionals. Having doctors who specialize in childhood diabetes will be important for maintaining the best healthcare possible for your child in the coming years. Introduce her to each of the doctors and tell her that the doctors are there to help keep her feeling healthy. Keep in close contact with the team, especially soon after being diagnosed, with any concerns, and with any major changes in your child's life. You may want to include: A pediatrician who is knowledgeable about childhood diabetes. A nurse who specializes in diabetes. A dietician. An endocrinologist, a doctor who specializes in hormone problems such as diabetes. A psychologist. The psychologist can help the child deal with the emotions caused by the diagnosis. Many children go through shock, anger, and denial before accepting the diagnosis.
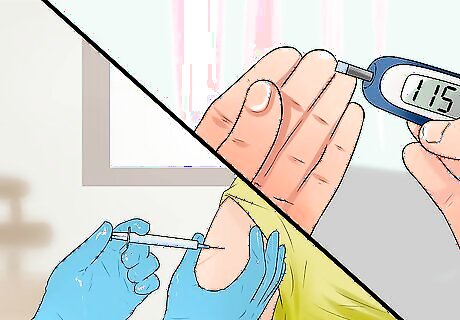
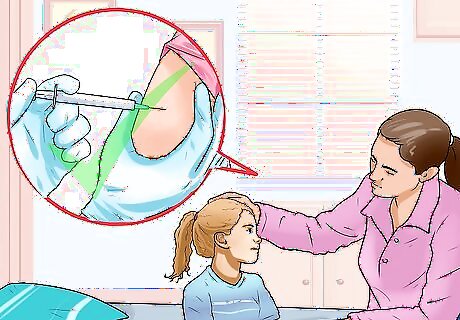
Practice blood sugar checks and insulin injections with your child. Be sure that they understand what is being done and why. This will make it less scary. If your child is old enough, allow him to practice doing the finger-prick test for measuring blood sugar and injections himself. If the child is too young to do the finger-prick test alone or give himself injections, you can involve him in the process by asking him to help pinch his skin during injections. This will help prepare him to inject himself when they are older.
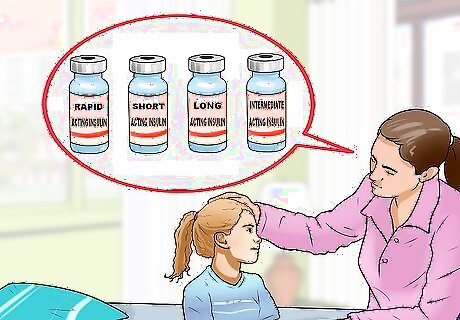
Explain about the different types of insulin. This will help your child understand the relationship between insulin and diet and help her to learn to manage it. Depending on your child’s needs, the doctor may recommend a mixture of different types. Insulin types include: Rapid-acting insulin. Two common ones are insulin lispro (Humalog) and insulin aspart (NovoLog). They take effect in 15 minutes or less and have their maximal effect at about one hour. Short-acting insulin (Humulin R, Novolin R, and others). This usually takes 30 minutes to work and has its greatest effect two to four hours later. Long-acting insulin. Common ones include insulin glargine (Lantus) and insulin detemir (Levemir). It is effective for 20 to 26 hours. Intermediate-acting insulin (Humulin N, Novolin N). This takes effect after half an hour and peaks in four to six hours. Children on this type of insulin have to be sure to eat the correct amounts of carbohydrates at the right times because intermediate-acting insulin is prone to causing low blood sugar.
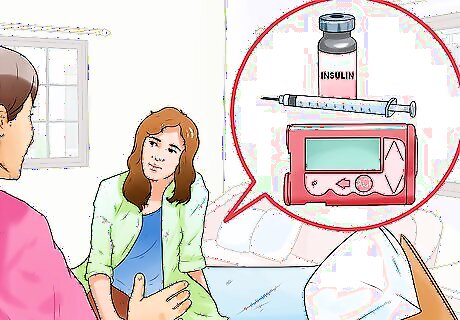
Allow your child to choose the delivery option, if they are old enough. Being able to discuss and understand the options may help your child take responsibility for his management plan. There are a few options available: Insulin injections. This option involves getting regular shots. The shots can be given with a needle and syringe or with an insulin pen. The pen has a container of insulin inside. An insulin pump. The pump is about the size of a deck of cards and it is worn on the body. It is attached to a catheter that remains continuously inserted under the skin. The pump is programmed to give insulin, but can be adjusted as needed. A wireless pump that uses small pods filled with insulin is a newer option.
Recognizing the Symptoms
Help your child recognize low blood sugar. Low blood sugar, also called hypoglycemia, can occur due to not eating enough, vomiting frequently, getting more exercise, or taking too much insulin. Teach your child to recognize the symptoms and to tell you when her blood sugar may be low. As they learn to recognize the symptoms, they will learn that managing her diabetes will lead to her feeling better. Symptoms include: Shaking Sweating Sleepiness Hunger Dizziness Headaches Bad mood Altered behavior Confusion Agitation Seizures Unconsciousness

Teach your child to identify high blood sugar. High blood sugar is also called hyperglycemia. It can be caused by eating more than usual, eating the wrong kind of food, not taking enough insulin, or being sick. As they start to recognize the symptoms of high blood sugar, they will understand that taking their medications is important for feeling good. Symptoms include: More frequent urination Thirst Dry mouth Blurry vision A yeast infection Exhaustion Nausea

Help your child recognize diabetic ketoacidosis. This occurs when the body begins to break down fat because it isn’t getting enough energy. You can teach your child to recognize the symptoms and to test for this condition using an over-the-counter kit to test her urine for high ketone levels. Symptoms of diabetic ketoacidosis include: Lack of hunger Nausea or vomiting Abdominal discomfort Dry or flushed skin Breath that smells sweet or fruity Confusion Fatigue Difficulty breathing or deep or rapid breathing
Helping Your Child Manage Diabetes
Work with your child’s school. As they get older, they will be responsible for managing their diabetes medication while they are at school. Whether this is giving himself injections or going to the school nurse’s office to be injected, it is important that they understand how his condition will be managed. Things to discuss with the school include: Introducing your child to the school health team. Make sure they know where the nurse’s office is so that if they feel unwell they can get help. Talking to your child’s teachers. Your child will need to always have a snack or quick-acting sugar source handy. Make sure the teachers are aware that they might occasionally need to leave class for insulin treatments or to have a snack. Asking your school how your child should dispose of used needles. If they are injecting themselves, they will need to know where to dispose of the needles safely.

Recognize if your child has needle phobia. It is not uncommon for young diabetics to develop a needle phobia. It can make the regular insulin injections extremely upsetting for both the parent and the child. Children with needle phobias may try to avoid getting injections or show the following symptoms of anxiety: Dizziness Dry mouth Heart palpitations Sweating Trembling Hyperventilating Fainting Nausea or vomiting
Help your child overcome needle phobia. There are several ways that this can be done. Your child may want to try different methods to see what helps. You may want to work with a psychologist familiar with the challenges children with diabetes face. Ask your child to create a fear hierarchy. As your child to make a list of the parts of the injection routine starting with the least frightening to the most frightening. Then start with the easy parts, like holding the syringe or watching someone else inject, and have your child do relaxation techniques until the fear subsides. Practice this until your child can work through the whole hierarchy. Teach your child to use relaxation techniques like deep breathing, meditation, visualizing calming images, or progressively tensing and relaxing different muscle groups in her body. Try injecting in different places, like a different room of the house or at a relative’s house. This may help remove the cues associated with the anxiety. Try injecting in different body parts. Many people find it less uncomfortable to inject in the stomach, but other options include the thigh or buttock. This may help if your child experiences soreness due to previous injections. Help your child find a support group. Your doctor may know of support groups for children with diabetes. You can also contact your local health center or search online with organizations that do diabetes education and outreach, such as Diabetes UK or the American Diabetes Association.
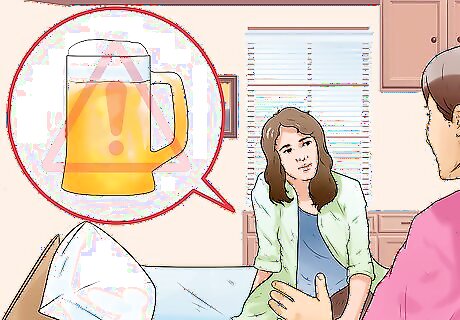
Support your teen as they gain independence. For teens with diabetes, the usual challenges of adolescence are more complicated. Maintain open communication with your teen and recognize that they may make mistakes. Teens are more likely to reduce compliance with their diet or insulin injections due to rebelling or trying to fit in with their friends. Possible challenges to discuss include: Driving. Talk to your teen about the importance of safety behind the wheel. Teach your teen to check her blood sugar before driving and to always keep non-perishable snacks in the glove compartment. Make sure they understand that it is always better to pull over and treat low blood sugar, even if it means being late. Tell her to be sure not to leave her diabetes supplies in the car because hot or cold temperatures may damage them. Body image. Some diabetics have trouble controlling their weight. If your teen is struggling with this, offer support. Teens are also at risk for eating disorders or skipping insulin in order to lose weight. Your teen may also wish to have confidential support from a counselor or support group as well. Alcohol. Alcohol can alter blood sugar levels. In addition, the awareness changes that occur when people are drunk can be similar to those with low glucose. Make sure your teen understands that alcohol may be particularly dangerous for her.














Comments
0 comment