
views
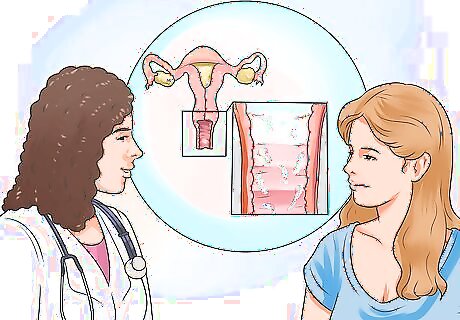
Getting a Diagnosis

Look for symptoms of bacterial vaginosis (BV). If you suspect you have a vaginal infection, pay attention to your symptoms. Not all women with BV have symptoms, but the following symptoms are often associated with BV: Vaginal discharge with an unpleasant or "fishy" odor Yellowish discharge Burning or discomfort when urinating Itchiness and irritation in and around the vagina
Pay attention to signs of a yeast infection (candidiasis). The symptoms of a yeast infection are similar to BV. They include: Abnormal vaginal discharge which can range from a thin, watery, white discharge to a thick, white, and chunky discharge (often described as looking like cottage cheese) Itching and burning of the vagina and labia Painful intercourse Painful urination Redness and swelling of the area just outside of the vagina.
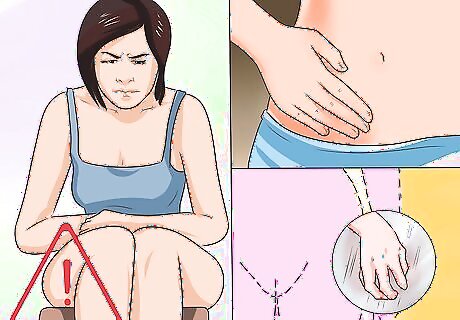
Look for signs of a trichomoniasis infection (trich). While many people with a trich infection have no symptoms, these symptoms are signs of an infection: Vaginal discharge that is smelly, frothy, bubbly, or foamy Vaginal itching Yellow or gray-green discharge Painful urination
Consider the cause of your bacterial infection. There is not always a specific cause for BV or a yeast infection other than a bacterial imbalance. Trich is an STI that is caused by a protozoan parasite called Trichomonas vaginalis. Most women have probably had at least one bacterial infection. The risk of getting BV increases with a new sexual partner (or multiple partners), douching, having sex without a condom, or using an intrauterine device (IUD) as a method of birth control. If you are diagnosed with trichomoniasis, you'll need to inform any sexual partners so they can be treated. Yeast infections and BV can be caused by antibiotic use. Antibiotics disrupt the normal balance of bacteria in your vagina which can allow "bad" bacteria or yeast to thrive. Other causes may include: wearing tight underwear or non-cotton panties (which can increase the temperature around the vagina and increase the moisture levels), a weakened immune system, using vaginal douches or perfumed feminine hygiene sprays, or vaginal trauma (scratches in the vagina caused by inserting objects like tampons or during rough sex). You should also tell any sexual partner about any vaginal infection, but you aren't required to.
Know when to get medical attention. Since different infections often have similar symptoms, it's critical that your doctor make a diagnosis so you get the correct treatment. See your doctor if you have any symptoms of a vaginal infection. Your doctor will prescribe a course of treatment, but if you don't notice an improvement after three days, have a fever, if the discharge symptoms worsen, or a new rash appears anywhere on your body contact your doctor. Keep in mind that recurrent yeast infections can be a sign of a more serious underlying disorder such as diabetes, cancer or HIV-AIDs. Recurrent yeast infections might suggest there's a problem with your immune system.

Get a physical examination. At the doctor’s office, your physician will probably take a sample of the vaginal discharge, ask for a urine sample and perform a vaginal exam. This exam may be uncomfortable but it is usually over quickly. The discharge will be tested for the presence of bacteria, yeast or other organisms such as Trichomonas. Your doctor will also ask about your sexual history, menstruation, vaginal hygiene, and any medications you're taking.
Learn how to handle recurring infections. Since different types of vaginal infections are treated differently, it's critical to get the correct diagnosis from a doctor before you start any treatment. Usually, after your first vaginal infection, you'll be able to tell when you have an infection, but it's still important to find out the type of infection. Untreated or incorrectly treated bacterial infections can cause complications like pelvic inflammatory disease (PID), pre-term births and low-birth weight babies and can put a woman at higher risk of sexually transmitted infections such as HIV, herpes simplex virus (HSV), chlamydia and gonorrhea. Untreated or incorrectly treated trichomoniasis infections can also lead to increased risk of HIV.
Treating Vaginal Infections

Take medication. Your doctor will recommend a course of treatment once your vaginal infection is diagnosed. Treatment will depend on the type of infection, how extensive or severe it is and how long you have had the infection. These are typical treatments for: Bacterial Vaginosis: Antibiotics like metronidazole or clindamycin. These are considered safe if you are pregnant. Male partners usually don’t need treatment, but female partners should be informed and tested. Yeast Infection: Antifungal creams, ointments, oral dose of fluconazole, or vaginal suppositories. Examples of these treatments are butoconazole, clotrimazole, miconazole (sold under the brand name Monistat) and terconazole. Your doctor can prescribe them or they are available (in weaker doses) over-the-counter at your pharmacy. Recurrent or more complicated yeast infections: Higher doses of medications used to treat yeast infections or you may be told to take them for a longer period of time. Since your partner may be the source of your recurring yeast infections, your partner may need to be treated as well. Trichomoniasis: A single dose of either metronidazole or tinidazole. These antibiotics are also considered safe if you are pregnant. Trichomoniasis is an STI, so make sure your sexual partner(s) are treated as well. You should wait for 7 days after treatment before you resume sexual activities.

Avoid douching. Douching is the procedure of washing or cleaning out the inside of the vagina with water or other fluids. Douching isn't recommended because the vagina naturally cleans itself and douching can increase the risk of bacterial infections. Douching can actually introduce bacteria, causing vaginal infections and other serious infections like pelvic inflammatory disease. There are no known methods to reduce your risk of infection from douching.

Eat yogurt. If you have recurrent bacterial infections, consider getting probiotics through yogurt. Probiotics can be effective in preventing future infections. Eat 150 grams of yogurt that has 4 to 5 billion Colony Forming Units (CFU) every day. Make sure to read the label for this information. While more research is needed, some studies suggest that bacterial cultures in yogurt or probiotic supplements can populate the vagina. Do not insert yogurt into your vagina.
Recovering From and Preventing Vaginal Infections

Know when to go back to the doctor. Contact your doctor if your symptoms don't improve, if you develop a fever, have difficulty or pain when you urinate, have painful sex, or experience abdominal pain. You should always inform your doctor when using natural treatments. Usually, you can take oral medications while using the natural treatments.

Keep the area clean. Use a very mild soap and warm water to wash your genital area. Dry yourself with a clean towel or air dry. You can also try drying the area with a blow dryer set on cool. Avoid bubble baths, bath oils, talc, or powder (especially powder which contains cornstarch). These can irritate the area and provide food for infection-causing microorganisms.
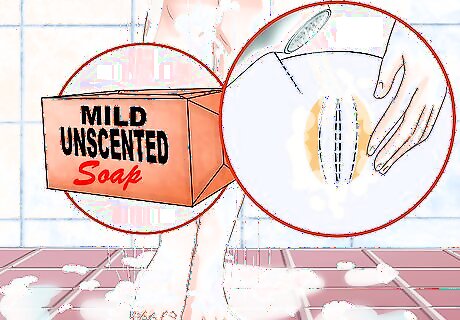
Avoid fragrances and irritants. Use a mild and fragrance-free soap for washing your panties. It's a good idea to double rinse your underwear. This ensures that all the detergent is gone. Do not use fabric softeners or dryer sheets since they contain chemicals that may irritate your vagina. Don't use feminine hygiene products, which can irritate the vulva. These include deodorant sanitary pads, all feminine sprays and deodorants, any products containing petroleum jelly, oils or greases.
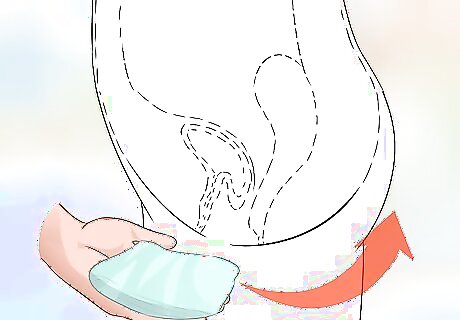
Practice good hygiene. After using the restroom, use white, soft toilet tissue and remember to wipe from the front. This minimizes the risk of infection from bowel bacteria. If you use tampons during the day, replace them every few hours depending on your flow and avoid using tampons with fragrance. Do not leave tampons in overnight. Use sanitary pads instead.
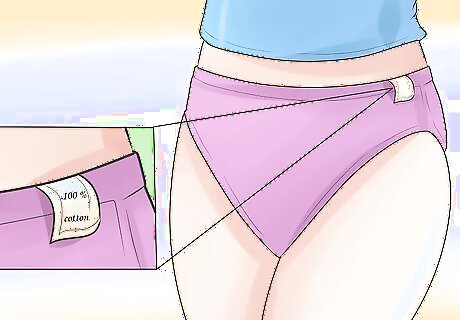
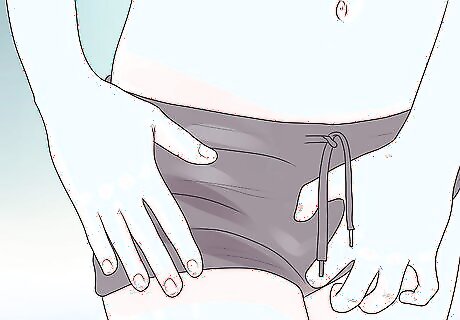
Wear non-irritating underwear. Choose white, 100 percent-cotton underwear. Cotton allows your genital area to stay cool and dry. The white underwear avoids irritants that may be in different dyes. Avoid underwear made with nylon, acetate or any synthetic fibers. You should also avoid wearing thong underwear which can irritate the genital area. Once you feel comfortable with the volume of your discharge, consider sleeping without underwear. This can be especially helpful for if you get recurrent BV. Avoid scratching or rubbing your genitals. Avoid wearing pantyhose. These trap heat and moisture which can allow bacteria, yeast and other organisms to thrive. Instead, wear nylons with a cotton panty insert.















Comments
0 comment