views
Basic Precautions
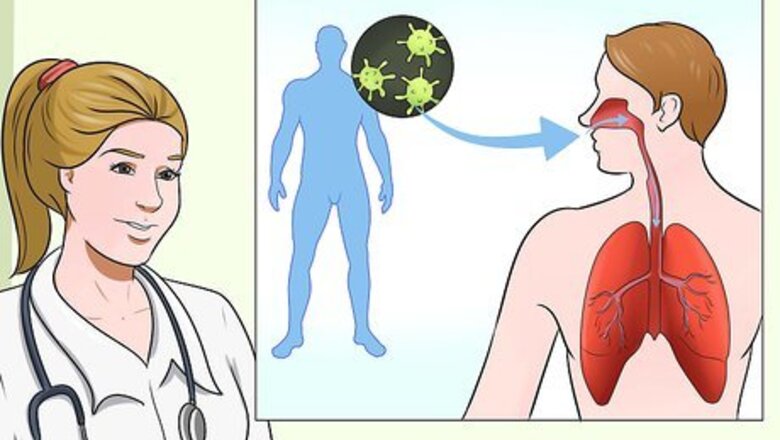
Understand how the chickenpox virus spreads. The virus is highly contagious and spreads in the air through particles that come from the lesions (sores) on the skin or from the upper respiratory tract. You can also get the virus if you touch the open lesions on an infected person and then touch your face, nose, or mouth. The disease takes 10 to 21 days (15-16 days, on average) after exposure to develop. If you’re in close contact with someone who has chickenpox and you don’t have immunity, there’s about a 90% chance you’ll get it. The person with the virus is contagious from 1 to 2 days before the rash breaks out on the skin and will continue to be contagious until ALL the lesions have crusted over. This typically happens around 5 days after the rash first appears. Some people who get vaccinated may suffer from breakthrough varicella, which is a mild form of the chickenpox that includes a rash of less than 50 lesions and a slight fever. These individuals are also contagious. However, those with breakthrough varicella are only one third as contagious as those who were not vaccinated.
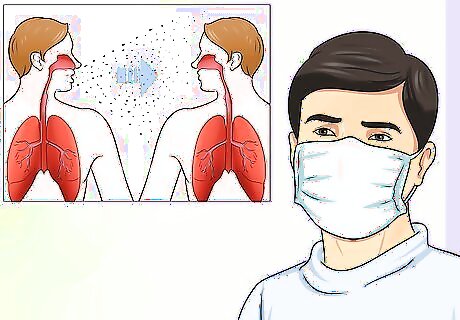
Wear a mask to protect yourself from droplet transmission. Take precautions when caring for an individual with chickenpox to reduce the risk of droplet infection. Wear a facemask to prevent secretions from entering your mouth and nose. A facemask should always be worn before being in the same room with the patient and a new mask should be used each time you wear one. Wear gloves, a gown, and goggles or a face mask if the individual is sneezing, coughing, or producing a lot of nasal secretions. Droplets from a sneeze can travel through the air for up to 200 feet, so it is crucial to protect yourself. The varicella zoster virus is spread through droplet transmission or from direct contact with the individual or touching objects or clothing that were in contact with the infected individual. Droplets may come from a sneeze, cough, speaking, nasal secretions, and saliva.
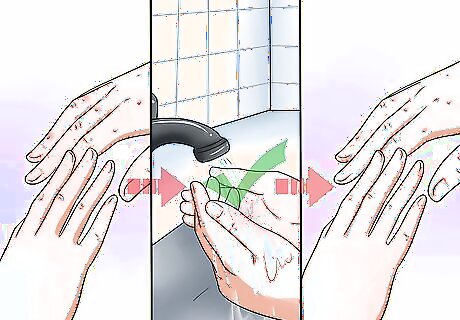
Wash your hands before and after touching the patient. Make sure that you wash your hands before and after touching the patient or after having any contact with the objects, materials, or secretions of the patient. Use soap and warm water to wash your hands. Lather your hands with soap and warm water for at least 20 seconds. Be sure to scrub the backs of your hands, between your fingers, and under your nails. If you need a timer for 20 seconds, hum “Happy Birthday” to yourself twice. Rinse your hands well under warm water and pat them dry with a clean towel or use hot air to dry them.

Keep the patient in one room to prevent the virus from spreading. The patient’s bedroom is often the best room. If possible, have the patient use only one of the bathrooms in the home and be sure that no other person in the home uses that bathroom. Have the patient put on a mask when they leave the bedroom to go to the bathroom. Any sneezing or coughing while out of the room may also spread the virus.

Use contact precautions for extra protection. Contact precautions include wearing a gown and gloves for any physical contact with the individual or other inanimate objects that may have had contact with the patient. When changing the bed sheets, entering the room, touching the patient, or handling any other objects, make sure that you are wearing goggles, gloves, and a gown.
Chickenpox Vaccination
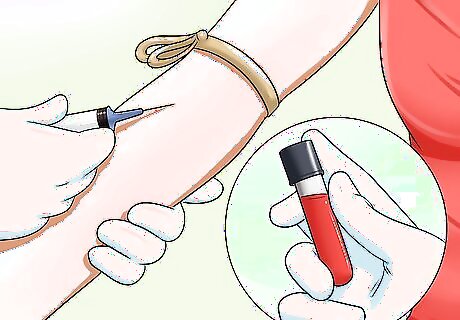
Get tested for immunity if you’re not sure you’ve had chickenpox. If you don’t remember whether you had the chickenpox or not, you were born after 1980, and you do not have family members who can remember, your doctor can draw a blood titer. This is a blood test that measures the antibodies in your blood for the chickenpox virus. If you were exposed to the chickenpox and had the illness, even if it was a very mild case, then you will have antibodies in your blood that will protect you from getting it again.
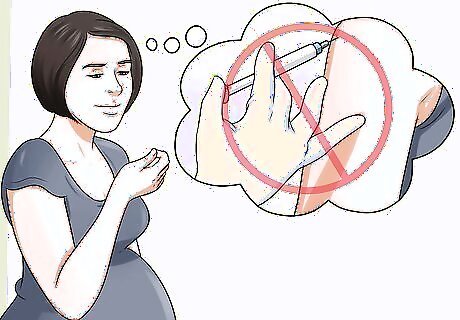
Talk to your doctor about whether the vaccine is safe for you. There are some people who should not have the vaccine to protect from chickenpox because of other medical issues. Discuss your medical history with your doctor to determine if you should not have the vaccine. In general, you should not get the vaccine if you: Have had an allergic reaction to the first dose of the vaccine Are pregnant Have allergies to gelatin or neomycin Have an immune system disease, such as HIV/AIDS Have received a high dose of steroids or other medications that affect your immune system Are undergoing any treatments for cancer with radiation, drugs, or chemotherapy Have had a transfusion or received blood products within the last 5 months
Ask about getting vaccinated if you’re not immune. Getting vaccinated against the chickenpox can also protect you from contracting the disease. Although most research has been done on vaccinations prior to exposure to the virus, vaccination after exposure does offer some effective protection. However, it is important to get the vaccine within 3-5 days of exposure to the illness for the best results. If you have not had the chickenpox nor received the vaccination, speak with your physician about being vaccinated. Some people who get the vaccine will get a mild case of chickenpox with fewer blisters than normal and often no fever at all. The vaccine is made from live or weakened viruses. Children get the vaccine at 12-18 months and another dose between 4 to 6 years old. The most common side effects of the vaccine are pain, redness, or swelling at the site of the injection. A small percentage of the children and adults who get the vaccine will also develop a mild rash around the spot where the shot was given.
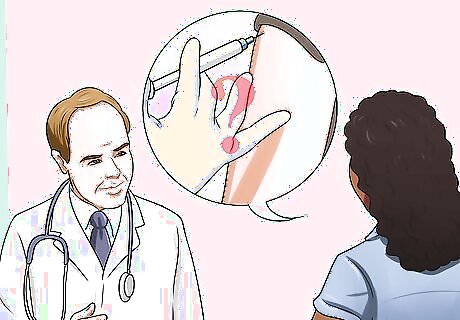
Look into taking immune globulin if you can’t take the vaccine. Even if you can’t have the chickenpox vaccine because of a health problem or concern, there are still other options. Ask your doctor about getting a varicella-zoster immune globulin treatment if you think you’ve been exposed to chickenpox. This treatment will help boost your immunity by giving you the antibodies you need to fight the virus. Try to get the immune globulin treatment as soon as possible after you’ve been exposed, and don’t wait longer than 10 days after the exposure. It won’t work as well if you wait too long. You’ll get this medication as a shot, just like the vaccine. Let your doctor know if you have any serious health conditions, such as heart disease or a history of blood clots or stroke. Also tell them if you’ve recently had a vaccine, since this treatment can reduce the effectiveness of some vaccines.
Discuss taking an anti-viral medication if you’re at high risk of getting very ill. If you’ve been exposed to the chickenpox virus and your doctor thinks you could get seriously ill, they might recommend a medication like acyclovir or valacyclovir. These medications could make your symptoms milder and help you recover faster. Ask about taking an antiviral medication if you’ve just started showing symptoms of chickenpox and: You’re older than 12 years old and aren’t immune to chickenpox You have a chronic health problem, such as heart disease You’re taking steroids or salicylate medications
Risk Factors and Treatment Options
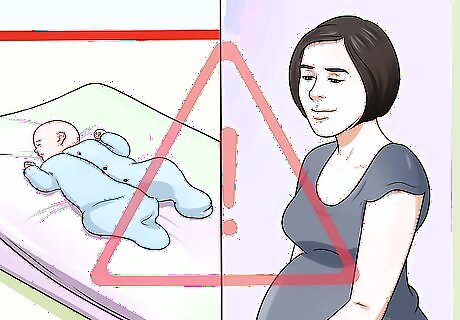
Recognize the risks for specific populations of people who get the chickenpox. There are several populations of people who are at higher risk of developing significant complications that can be life threatening. These people include: Newborns and infants whose mothers have not had the chickenpox or the vaccine Adults Pregnant people who haven’t had the chickenpox People whose immune systems are impaired by medications People taking steroids People with health conditions that affect their immune system, such as cancer or HIV/AIDS. People with HIV infections sometimes develop chronic chickenpox.
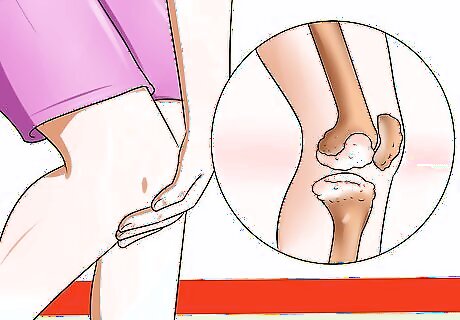
Be aware of the potential complications associated with severe chickenpox. In some cases, the chickenpox can have serious complications that require emergency medical interventions. Complications from varicella infections include, but are not limited to: Bacterial infections of the skin or soft tissue Pneumonia Septicemia (infection in the blood) Toxic Shock Syndrome Bone infections Septic arthritis (joint infection) Encephalitis (inflammation of the brain) Cerebellar ataxia (inflammation of the cerebellum in the brain) Dehydration Joint infections
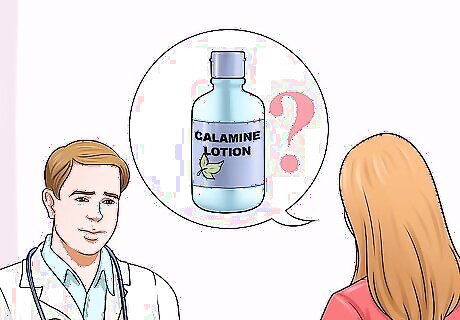
Discuss treatment options with your doctor. Treatments for the chickenpox are usually supportive and done at home. If you are at higher risk and develop other conditions with the chickenpox, then you may need hospitalization for treatment of the secondary infection and supportive therapy. At home treatments will help the individual to recover more comfortably. Common at home treatments for the chickenpox include: Calamine lotion and colloidal oatmeal or baking soda baths to help dry out the lesions and relieve the itching. Benedryl, which can help reduce itching and inflammation. For adults, the typical dose is 25-50mg 3 times a day. If you’re treating a child, ask your doctor to recommend a dose based on the child’s weight. Non-aspirin medications, such as acetaminophen, to relieve fever. Aspirin products can sometimes cause a severe, life-threatening reaction in children and teens called Reyes syndrome, so never give aspirin or other medications with salicylic acid to a child. Antiviral medications for people in a high-risk group who may develop secondary infections. Those antiviral medications include acyclovir, valacyclovir, and famciclovir.
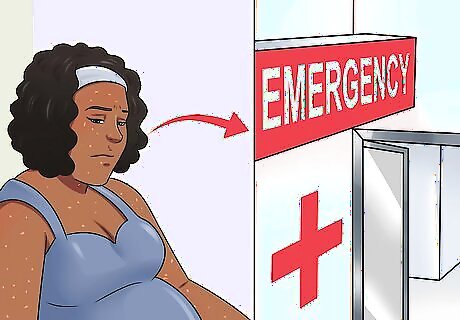
Know when to seek medical attention. If the individual is being treated at home, it is important to know what situations require immediate medical attention. Call your doctor or take the individual to an emergency room if the individual: Is older than 12 years of age for preventative supportive care Has a weakened immune system Is pregnant Has a fever that lasts longer than 4 days Has a fever above 102 °F (39 °C) Has areas of the rash that become very red, warm, or tender Has an area that leaks thick discolored fluid Has difficulty waking up or appears confused Has difficulty walking Has a stiff neck Has frequent vomiting Has difficulty breathing or a severe cough













Comments
0 comment