
views
The focus of the government towards promoting the overall well-being of women has started bearing fruits. The convergence of several government schemes and policies are gradually impacting the lives and is providing the much-needed freedom of decision-making to women. Whilst the ‘Beti Bachao, Beti Padhao’ (Save the girl, Educate the girl) initiative is thriving on the broader vision of gender equality, addressing the declining child sex ratio, promoting education and empowering girls; Pradhan Mantri Ujjwala Yojana scheme — aimed to provide free LPG connections to women from below-poverty-line families — is promoting clean cooking and improving health. Similarly, Sukanya Samriddhi Yojana, a savings scheme for the girl child, is encouraging parents to save for their daughter’s future and Swachh Bharat Abhiyan — while not exclusive to women — is campaigning for clean sanitation facilities. This has had a significant impact on the health and dignity of women.
While the Indian government has made commendable efforts to prioritise women’s issues, there still remains a critical need for intensified focus on women’s health. Addressing prevalent health issues such as anaemia, and malnutrition, and concerted efforts towards combating prevalent non-communicable diseases, including breast and cervical cancers, is much needed. Screening programs and awareness campaigns can contribute to early detection and improved outcomes.
Breaking Barriers: Battle Against Cervical Cancer & Anaemia
With annual mortality of over 916,827 and an incidence of over 1.4 million, cancer has rapidly grown into one of the leading drivers of mortality and morbidity in India. Late detection and inadequate access to quality treatment imply that outcomes are despairingly poorer as compared to developed countries. Not surprisingly, even cancers such as those of breast, cervical and oral that are amenable to screening and early detection account for over 33 per cent of the incidence and 28 per cent of the mortality.
The challenges vis-à-vis cervical cancer are even more acute. With an incidence of approximately 127,526 and a mortality of over 79,906 in 2022, it is the second leading cause of cancer amongst women, accounting for 17.7 per cent of cancer burden (by incidence). Poor awareness and knowledge gaps, limited geographic (limited availability and concentration of cancer services) and economic access (low insurance penetration and high cost of treatment in the private sector) to quality screening and treatment services, further magnified by gender-related issues and privacy concerns, are significant barriers in accessing care.
In India, the overall pooled data of cervical cancer five-year survival (between 2012 and 2015) was 51.7 per cent. The number of cervical cancer cases prevalent for five years is approximately 339,589 women. The National Sample Survey’s (NSS) 75th round conducted during July 2017-June 2018 revealed an alarming picture associated with cancer care in India. Based on data recently released, at the national level, average total cancer care expenditure was around Rs 1,16,218 and 93 per cent of this (Rs 1,08,659 out of Rs 1,16,218) is out-of-pocket (OOP) expenditure. Late-stage diagnosis is common due to limited awareness and healthcare infrastructure, leading to reduced treatment efficacy and higher mortality.
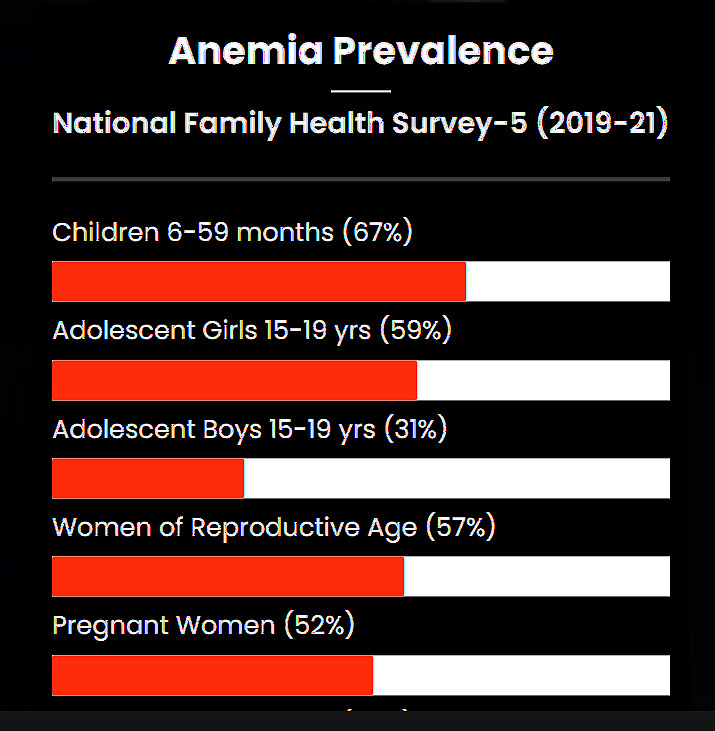
Globally, every fourth woman dying from the disease is Indian; we lose 218 women to cervical cancer every day in India. Whilst this is a matter of grave concern, we can’t ignore the elephant in the room – anaemia. Iron deficiency anaemia (IDA) continues to be a major public health problem in India and impacts the prognosis of cancer patients significantly. It is estimated that about 20 per cent of maternal deaths are directly related to anaemia and another 50 per cent of maternal deaths are associated with it. The question, therefore, is why, despite being the first country to launch the National Nutritional Aanaemia Prophylaxis Programme in 1970, the problem of IDA remains so widespread. As is to be expected, the economic implications of IDA are also massive. Furthermore, anaemia of chronic disease — the second most prevalent anaemia — is caused by iron deficiency which happens in patients with acute or chronic immune activation.
Cancer patients with anaemia also face emotional and mental costs in addition to lack of self-motivation, sorrow, frustration and mental collapse. Almost one patient with malignancy in two is anaemic, with the consequence of poorer treatment outcomes and quality of life. A low haemoglobin (Hb) level seems to directly affect treatment efficacy, predominantly of radiotherapy, probably due to low tissue oxygenation causing decrease in radio-sensitivity. Tissue hypoxia might also enable tumour progression and impair the efficacy of cytostatic drugs.
The world is continuously combating this problem despite the fact that these problems are largely preventable and easily treatable. Cervical cancer has a long pre-cancerous window during which it can be identified, and pre-cancerous lesions treated, thereby preventing progression to cancer. Screening and treatment of pre-cancerous lesions are amenable to decentralisation and can potentially be undertaken at primary and secondary-level facilities. In November 2020, the World Health Organisation (WHO) announced a global strategy to accelerate the elimination of cervical cancer as a public health problem. This, amongst other interventions, recommends that 70 per cent of women be screened for cervical cancer by 35 years of age, and to ensure that 90 per cent of women identified with cervical disease receive treatment.
Convergence chronicles: Interplay of cervical cancer and anaemia
Anaemia has shown increase in all age groups from 2015-16 to 2019-21, which impacts the overall lifecycle approach. While anaemia and cervical health may not have a direct causal relationship, they can be interconnected in several ways. Anaemia is a condition characterised by a lack of red blood cells or haemoglobin in the blood, leading to reduced oxygen-carrying capacity. Cervical health, on the other hand, often refers to the well-being of the cervix, particularly in the context of conditions like cervical cancer.
Anaemia and cervical health may be related in one or many ways:
Impact on Immune Function: Anaemia can compromise the immune system, making individuals more susceptible to infections, including those affecting the reproductive organs. This may indirectly influence cervical health.
Menstrual Irregularities: Anaemia is often associated with heavy menstrual bleeding, which can affect cervical health. Prolonged or heavy periods may increase the risk of certain gynaecological issues.
Nutritional Factors: Both anaemia and poor cervical health can be influenced by nutritional factors. Adequate iron levels are crucial for overall health, including the maintenance of healthy blood and tissues.
Reduced Oxygen Supply: Anaemia results in reduced oxygen delivery to various tissues in the body, and this can impact the health of cells, including those in the cervix. Oxygen is essential for cellular function and repair.
Health Disparities: Socioeconomic factors that contribute to anaemia may also be associated with limited access to healthcare services, which can impact cervical health. Initiatives like the National Rural Livelihood Mission may play a role in addressing these disparities.
It’s important to note that while these connections exist, addressing anaemia and promoting cervical health often involve distinct medical and public health strategies. Regular screenings for cervical cancer, maintaining a nutritious diet, and addressing anaemia through appropriate medical interventions are essential components of overall health and well-being.
Way Forward: NCD Screening and Anaemia Management in Cancer Patients
Regular screenings play a vital role in identifying cancer at its initial stages, enabling timely interventions and improved treatment outcomes (National Cancer Institute). As per NFHS-5, only 1-2 per cent of citizens of the country have ever undergone screening for oral, breast and cervical cancer. Given the government’s focus on screening 37 per cent of India’s population, add-on solutions are required to complement the efforts of the government.
Introducing ‘Digital Wellness Centres’ for non-communicable diseases (NCD) and anaemia testing to conduct the first level of screening will aid in risk stratification rather than age stratification of the population and effectively lead to reduced ramifications of these diseases. Additionally, risk stratification will reduce patient load and enable better quality screenings/services and improve disease outcomes.
Digital Wellness Centres – Social Enterprise by NRLM Members
The Economic Survey 2022-23 has a special mention of high-impact banking operations done by self-help group (SHG) members, leading to the disbursement of billions of rupees every year. As India boasts of 12 million odd SHGs, leveraging this platform is paramount towards seeding the concept of wellness in the community.
India grapples with a strained patient-nurse ratio, urging the incorporation of a parallel cadre, such as NRLM members, to emphasise holistic wellness. By diversifying roles, these members can proactively engage in preventive healthcare, reducing illness rates. This innovative approach not only optimises healthcare resources but also fosters a community-centric strategy in mitigating the burden on the healthcare system.
With concerted efforts and determination, the first Digital Wellness Centre was set up in Madhya Pradesh under a pilot project led by Karkinos Healthcare, Career Institute of Medical Sciences and Vishwanath Cancer Care Foundation (VCCF) with CSR support from LT Foods. Anita Ahirwar, a member of the consortium and a SHG member herself, believes that it has triggered conversations about individual and family well-being. They are not willing to be manipulated by the hands of the local quacks. She understands generic medication is capable of providing affordable healthcare services. Her group was identified as local brand champions and they believe more such centres can be set up if advocacy regarding anaemia and cancer is scaled up. Health entrepreneurship within SHGs is a powerful example of grassroots initiatives promoting healthcare access and economic independence.
Health clinics set up by NRLM members not only serve as a means to provide essential healthcare services but also present a sustainable business and revenue model case. By charging nominal fees for consultations (lifestyle and dietary diversity); anaemia, diabetes, and blood pressure checkups; these clinics generate revenue to cover operational costs and even reinvest in community development initiatives.
NHM Mandate: Integrating Ferrous Ascorbate for Cancer Patients
As India progresses towards comprehensive healthcare reforms, it is imperative for the government to address the pressing issue of anaemia in cancer patients. Iron deficiency remains one of the most widespread nutrient deficiencies globally, posing significant challenges to treatment outcomes, particularly in cancer care settings. Cancer patients are especially vulnerable to anaemia due to increased iron needs during treatment, exacerbating the severity of their condition.
To mitigate these challenges and improve treatment efficacy, it is essential for cancer treatment centres to integrate ferrous ascorbate supplementation alongside cancer therapies. Ferrous ascorbate, along with Carbonyl iron, emerges as a promising solution, offering enhanced efficacy and improved tolerability compared to conventional iron preparations like Ferrous sulphate and Ferrous fumarate.
By prioritising the implementation of ferrous ascorbate supplementation protocols in cancer care facilities, the government can significantly enhance the well-being and treatment outcomes of cancer patients. This proactive approach underscores the importance of addressing anaemia as an integral component of holistic cancer care, ensuring that patients receive comprehensive support throughout their treatment journey.
Kausar Kidwai, Assistant Vice President, Karkinos Healthcare Private Limited has been extensively working in the healthcare domain (public and private sector) with focus on disease prevention strategies. Views expressed in the above piece are personal and solely those of the author. They do not necessarily reflect News18’s views.
















Comments
0 comment